New Metric Determines Adequacy of VA Primary Care Staffing
BACKGROUND:
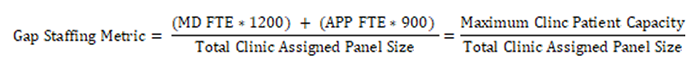
Improving patient access to care necessitates balancing patient demand with provider availability. "Panel size" (i.e., the number of patients a primary care provider (PCP) is responsible for), is associated with patient satisfaction, provider burnout, clinical quality, access, and efficiency. In VA primary care (PC), PCPs lead four-person Patient Aligned Care Teams (PACTs) that include a nurse care manager, a clinical associate, and an administrative clerk. PACTs have a panel size of 1,200 patients per 1.0 full-time equivalent (FTE) physician-led team and 900 patients per 1.0 FTE APP (Advanced Practice Provider)-led team. This study created a PCP staffing measure using clinic-level provider FTE and number of assigned patients to identify PC clinics at risk of insufficient staffing and describe rural-urban staffing variation. Using VA administrative data from 2017-2021, investigators created the following equation to calculate a monthly gap-staffing metric in 916 VA PC clinics.
FINDINGS:
- Over the 3.5-year study period at the 916 clinics, 38 (4%) were always under-staffed, 21 (2%) were always marginally staffed, and 200 (22%) were always fully staffed.
- At the end of the study period (March 2021), 351 PC clinics (39%) were not fully staffed and 179 of these clinics (51%) had a gap of at least 0.5 APP FTE, representing a potential minimum threshold for hiring a new provider. But 559 clinics were fully staffed with excess clinic capacity of 11-15%.
- Depending how FTE is distributed (e.g., across clinics vs. within each clinic) and the provider type, 228 to 521 PCP FTE are needed to fully staff all PC clinics as of March 2021. This represents a 4-8% provider staffing deficit.
- Over the entire study period, rural clinics, on average, were under-staffed for 21% of months compared to 14% of months for urban clinics, a 50% higher rate.
IMPLICATIONS:
- The gap staffing metric may be a beneficial tool to identify PC clinics that are persistently over- or under-staffed, facilitating strategic workforce planning and allowing better distribution of provider FTE to address patient care needs.
LIMITATIONS:
- Calculations used in this study depended on data accuracy, including VA provider FTE and assigned patient data.
AUTHOR/FUNDING INFORMATION:
This study was partly funded by HSR&D. Drs. O’Shea, Shahnazi, and Kaboli – and Mr. Haraldsson are part of HSR&D’s Center for Access and Delivery Research and Evaluation (CADRE). Drs. Sterling and Wong are with HSR&D’s Denver/Seattle Center for Veteran-Centered and Value-Driven Care.
O’Shea A, Haraldsson B, Shahnazi A, Sterling R, Wong E, and Kaboli P. A Novel Gap Staffing Metric for Primary Care in the Veterans Health Administration and Implications for Rural and Urban Clinics. The Journal of Ambulatory Care Management. August 4, 2022; online ahead of print.