
|
|
Research HighlightA Learning Health System Approach to Using Artificial Intelligence Enabled Decision Support (AEDS) for Medication Optimization in Veteran Care: An Immunosuppressants Use CaseKey Points
In the modern era of drug development, our healthcare system faces growing resource challenges. Drug manufacturers regularly introduce novel, resource-intensive treatments requiring outpatient services (e.g., access to specialists and infusion centers). The Veterans Health Administration (VHA) must provide high-quality care in the context of: (1) competing resources (e.g., specialist shortages, limited infusion services); (2) health system stressors (e.g., COVID-19 pandemic); (3) the incremental benefit of novel medications over established treatments; and (4) the needs of Veterans (e.g., driving distance, wait times). VHA faces a critical need and opportunity to both optimize treatment with established medications to maximize their benefit and provide high-quality care while also considering competing VHA resources and Veterans’ needs. This challenge is exemplified in the treatment of inflammatory bowel disease (IBD), which is a chronic, often debilitating immune-mediated disease. IBD consists of Crohn’s disease (CD) and ulcerative colitis (UC), and affects nearly three million Americans and approximately 80,000 Veterans.1 An estimated $8.5 billion dollars is spent annually on IBD medications, driven primarily by novel biologics (~$20,000 per patient per year on average, likely higher), whereas traditional immunosuppressants (thiopurines) are much less costly (<$200 per patient per year).2 Yet, current approaches to care still result in persistent symptoms and complications, indicating an urgent need to optimize IBD medications for our Veterans. One approach to medication optimization is to augment clinical decision-making using Artificial Intelligence (AI)/Machine Learning (ML)-based prediction models within a decision-support system (DSS). These AI/ML-enabled DSS (AEDS) can be integrated into healthcare using a learning health systems conceptual framework that focuses on model development (Data-to- Knowledge), intervention development and acceptability (i.e., AEDS; Knowledge- to-Practice), and impact evaluation (i.e., impact on clinical outcomes, resources, etc.; Practice-to-Data). This approach can be applied to medication optimization for Veterans with IBD and other conditions. Thiopurines are widely used to treat Veterans with immune-mediated conditions. In IBD, they are used alone (primarily UC) or in combination with a biologic (UC and CD), yet optimal thiopurine treatments for IBD are challenging. First, treatment response and adverse events vary by patient, suggesting a need for a personalized approach. Second, provider uptake and approach to thiopurine optimization varies widely, suggesting the need for clinical decision support. To address these needs, we developed an AI/ ML-based model that leverages electronic health record (EHR) data to predict whether an IBD patient on thiopurines is inadequately immunosuppressed.3 The model is highly accurate and precise and is currently deployed into an AEDS that provides an immunosuppression score to augment provider decision making for thiopurine dose optimization. However, the AI/ML-based prediction model has not been validated in a Veteran cohort (older, predominately male) nor in patients on combination therapies (thiopurines + biologic). We also lack a clear understanding of the barriers to successful implementation and adoption of an AEDS in VHA and a benchmark to compare how AEDS impacts clinical outcomes. The overarching goal of this project is to address these needs by using a learning health systems framework (Figure 1) with the long-term goal of deploying and adopting AEDS for medication optimization in VHA. We will (1) adapt and validate AI/ML-based models to predict non-remission (inadequate immunosuppression) in Veterans with IBD using real-world data from the VHA EHR (Data-to-Knowledge); (2) assess the usability, acceptability, and feasibility of AEDS for thiopurine optimization in Veterans with IBD (Knowledge-to-Practice); and (3) evaluate an AEDS-based treatment policy vs. usual care on clinical outcomes in Veterans using reinforcement learning (Practice-to-Data). 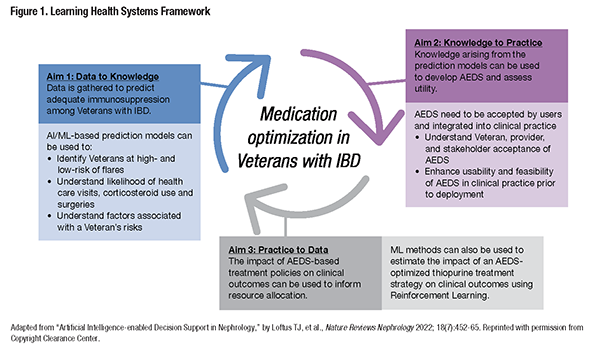
References
|
|