|
» Back to Table of Contents
Artificial intelligence (AI) has emerged as a transformative force across multiple industries and sectors, including healthcare. Rapid advances in AI present new opportunities for research and development (R&D). The Department of Veterans Affairs – home to the largest integrated healthcare data system in the country – has a particularly important role in fostering AI healthcare R&D to better serve Veterans, while simultaneously managing the evolving risks that are inherent in narrow and generative AI.
A recent study conducted by the VA Office of Research and Development examined AI R&D activities overall in VA, compared with those of other similar federal institutions. What type of AI research is done? How do different agencies compare in their pursuit of AI research? Where are there gaps and opportunities? Our analysis examined the corpus of AI R&D in VA, NIH, and other Non- Public Health Service agencies such as the National Science Foundation (NSF). This article summarizes our results and identifies potential opportunities for future VA R&D.
We collected all publications from PubMed between 1985 and 2024, specifically those with Medical Subject Headings (MeSH) terms relating to “Machine Learning and Artificial Intelligence in Healthcare.” We then identified whether the articles were published by VA, NIH, or other Non-Public Health Service agencies (Non-PHS) such as NSF. Furthermore, we used language models to identify coherent themes across these publications so that we could disaggregate the broad topics.
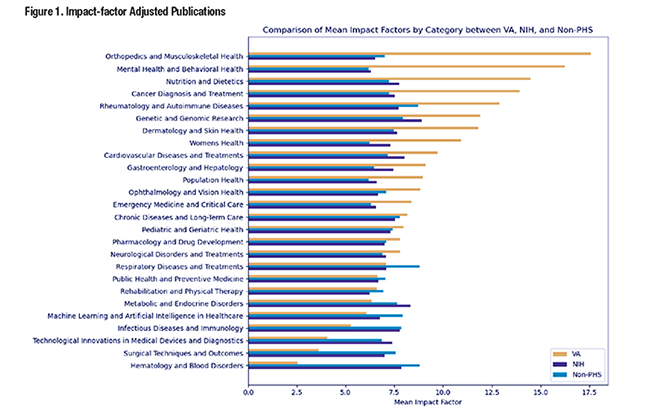
Figure 1 summarizes the results of our study, illustrating the differences in AI research topics across the three groups (VA, NIH, Non-PHS).
Below, we summarize three key takeaways from our study.
- Articles related to AI R&D in the area of novel methods in machine learning and artificial intelligence in healthcare represented a greater proportion of NIH (30 percent) and Non-PHS (40 percent) publications, compared with the proportion of VA publications (19 percent).
- Papers related to AI R&D in the area of public health and preventive medicine constituted a greater proportion of VA papers over the study period (9 percent) when compared to NIH papers (5 percent) and Non-PHS (5 percent) papers.
- AI R&D in the area of rehabilitation and physical therapy is a strong focus for VA (6 percent) compared to NIH (2 percent) and Non-PHS (3 percent). VA also shows notable engagement in respiratory diseases, men’s health, and cardiovascular diseases compared to NIH and Non-PHS publications. VA’s focus on cancer diagnosis and treatment is lower than NIH’s, but higher than among Non-PHS agencies.
We also looked at journal impact factors, which revealed the following differences.
- Cancer diagnosis and treatment publications involving AI R&D: VA’s research (mean journal impact factor 14) is larger than NIH (8) and Non-PHS (7).
- Dermatology and skin health involving AI R&D: VA again leads with a higher mean impact factor (12) compared to NIH (8) and Non-PHS (7).
- Genetic and genomic research involving AI R&D: VA’s work has a higher mean impact factor (12) than NIH (9) and Non-PHS (8).
- Mental health and behavioral health involving AI R&D: VA’s research is particularly impactful with a mean impact factor of 16, surpassing that of NIH (6) and Non-PHS (6).
To find areas of greatest potential synergy in VA for AI R&D, we analyzed the content of leading publications and overlayed it with our preceding analysis. Our analysis identified the following R&D opportunities.
- AI Diagnostics
One of the most prominent trends in the field of AI and machine learning is its potential use in healthcare diagnostics. Examples include AI-based symptom checkers that enable patient-centered tools (VA) and models for prostate cancer detection (VA) or cardiovascular disease prevention (HHS/NIH). These models rely heavily on unsupervised and supervised learning techniques to aid in personalized healthcare. Another significant trend is the increasing integration of deep learning into medical imaging, such as MRI and CT scans. AI can improve imaging accuracy and enhance diagnostic precision in clinical settings.
- Neuroscience and Cognitive Health
Brain-computer interfaces (BCI) represent another prominent area of AI innovation, as seen in VA’s work on robotic arm control using tactile Additionally, Amygdala-hippocampus subnetwork studies (Non-PHS) use neural networks to understand human mood and behavior. Furthermore, papers exploring spatiotemporal dynamics (HHS/NIH) and cortical neuron trajectories (Non-PHS) show how machine learning can be used to decode complex brain behavior, affecting treatment for conditions like depression or improving motor control in individuals with neural impairments.
- AI for Personalized and Preventive Care
There is a growing trend towards genomics-driven medicine using AI. For instance, deep learning helps predict the impact of genetic variations on diseases like glioblastoma (VA), while other works explore genomic profiling in cardiovascular disease (HHS/NIH). We also find evidence of AI’s ability to improve preventive healthcare as illustrated by studies on early disease detection, such as NIH’s AI systems for stroke risk prediction and COVID-19 severity. These predictive models help reduce patient risk by enabling earlier interventions, a key aspect of modern AI in healthcare.
- Imaging and Bioinformatics
The use of deep learning to improve resolution, such as in microscopy (HHS/ NIH) or MRI (VA), has helped researchers uncover critical insights at the cellular or molecular level. Papers from VA and HHS/NIH frequently emphasize how bioinformatics powered by machine learning is transforming disease classification and treatment. miRNA-based classification of diseases like glioblastoma demonstrates the potential of AI in making complex biological data actionable.
- Ethical AI
As AI moves from small pilots to larger enterprise applications, there are increasing risks to manage around data security, model reliability, and particularly the possibility of “hallucinations,” instances where the language model generates fictional information and/or data in response to a query or other human-driven interaction. As a result, developing and adhering closely to ethical guidelines and regulatory frameworks is critical to ensure safety and reproducibility in AI applications (see our recent article in Health Policy OPEN, which provides a unified taxonomy for understanding trustworthy AI frameworks). Recent incidents with large language models, including the prevalence of hallucinations in clinical notes with transcription technologies in which the language model may construct a fictional response, underscore the necessity of instituting audit processes and review.
VA has made significant strides in advancing AI research, but gaps remain. Our topic modeling of all AI related publications across federal agencies identified areas where VA has had an advantage, as well as the areas that are emerging and pose opportunities for expanded AI R&D. These opportunities range from linking genomic information with medical records for personalized healthcare to the development of ethical AI guidelines that manage risk for patients and enterprises. Pursuing such work would ensure that AI technologies continue to benefit Veterans while managing the ethical and social risks associated with these technologies.
|
