
|
|
Research HighlightAccess, Quality, and Equity of Atrial Fibrillation Care in VAKey Points
Atrial fibrillation (AF) is the most common cardiac arrhythmia worldwide, affecting as many as 70 million individuals. The prevalence of AF is up to 6 million in the United States, a number that includes as many as 1 million patients cared for in VA over the past decade.1 AF is associated with increased mortality and morbidity, including congestive heart failure, coronary heart disease, and ischemic stroke, the risk of which increases by five-fold with AF. Oral anticoagulation (OAC) for non-valvular AF reduces stroke risk by up to 70 percent and is the standard of care for stroke prevention in AF. For decades warfarin was the only OAC therapy available, but its use was challenging. A newer class of direct oral anticoagulants (DOACs) with substantially fewer management challenges was initially approved by the U.S. Food and Drug Administration in 2010 and came into use in VA in 2011. Over time, DOACs, including apixaban, dabigatran, edoxaban, and rivaroxaban, have demonstrated superior clinical and cost effectiveness, safety, and adherence compared to warfarin. Despite the effectiveness of OAC, racial and ethnic inequities exist in the initiation of such therapy. In prior analyses by our research team using insurance claims and clinical registries, racial and ethnic minorities with AF were less likely than white individuals to be treated with any form of OAC, and DOACs, even controlling for patient sociodemographic and clinical characteristics.2 These disparities are particularly noteworthy given the fact that racial and ethnic minorities with AF also have higher rates of stroke and mortality than white individuals. VA provides an advantageous environment to examine treatment disparities, as it provides medications to its enrollees through a uniform national drug formulary. Our team thus set out to compare OAC initiation by race/ethnicity for patients with new-onset AF managed in VA. Developing our Study CohortIn 2019, we received pilot funding from the VA VISN 4 Competitive Career Development Fund to develop a cohort of Veterans newly diagnosed with AF from 2010 to 2018. The cohort, now referred to as the Race, Ethnicity and Anticoagulant CHoice in Atrial Fibrillation, or REACH-AF, began with 827,502 Veterans with an index AF diagnosis from 2010 to 2018. After several exclusions (for example, patients without continuous VA enrollment or with conditions limiting their use of oral anticoagulation therapy), our cohort included over 250,000 patients. As a final step, we excluded individuals who were diagnosed with AF before 2014, which was prior to when three of the most prescribed DOACs were available in VA, resulting in a cohort of 111,666 Veterans with newly diagnosed AF. Identifying Patient, Provider, and Facility Determinants of DisparitiesWe examined patient, provider, and facility-level characteristics that could be considered potential drivers of the association between race, ethnicity, and OAC/DOAC initiation. We used VA administrative data on race and ethnicity to define this variable as non-Hispanic White, non-Hispanic Black, Hispanic, Asian, or American Indian/Alaska Native (AI/AN). We identified several other baseline patient sociodemographic characteristics, including age at index diagnosis, sex, VA priority group, region, rurality, and area deprivation index. We then examined various clinical factors, including the validated CHA2DS2VASc stroke risk and HAS-BLED bleeding risk scores. Using VA clinic stop codes, we identified provider-level variables including the clinical site associated with the index AF diagnosis and whether there was a clinical encounter with a cardiologist within 90 days of the index diagnosis. We also assessed the VA clinical site where the index AF diagnosis was recorded, categorized as VA medical center or community-based outpatient clinic. Results from the REACH-AF CohortOf our final cohort, 98 percent were male and 86 percent were white. Other racial and ethnic groups were Black (9 percent), Hispanic (4 percent), Asian (2 percent), and AI/AN (0.5 percent). Overall, 69,590 (62 percent) patients initiated any OAC therapy, varying 10.5 percentage points by race and ethnicity; initiation was lowest in Asian (52 percent) and Black (60 percent) patients and highest in white (63 percent) patients. In our final model adjusting for all patient, provider, and facility factors, the adjusted odds of initiating any OAC therapy were significantly lower for Asian and Black patients (see Figure 1).3 Among those who initiated any OAC therapy, 45,381 (65 percent) initiated DOAC. DOAC initiation varied by 7.7 percentage points across race and ethnicity groups and was lowest in Hispanic (58 percent), AI/AN (60 percent), and Black (61 percent) patients and highest in white (66 percent) patients. In models adjusting for all patient, provider, and facility factors, the adjusted odds of initiating DOAC therapy were significantly lower for Hispanic, AI/AN, and Black patients. 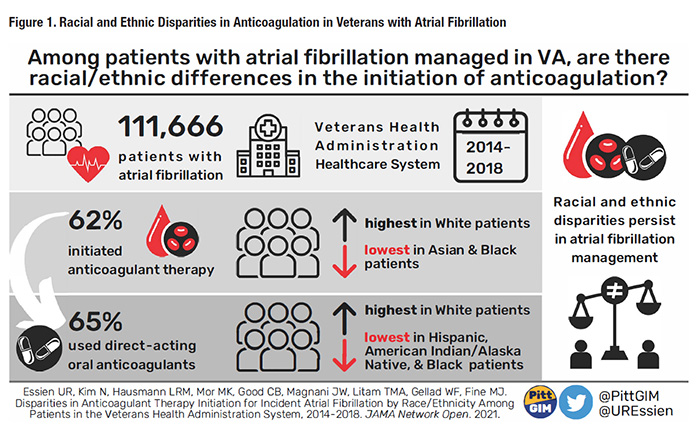
The Path Forward – Ensuring Equitable AF CareIn our national VA study, we found that Black and Asian patients were significantly less likely than white patients to initiate any OAC; among those who initiated OAC, Black, Hispanic, and AI/AN patients were significantly less likely to initiate DOACs. These findings were noteworthy given VA’s uniform drug formulary and low-to-negligible medication co-payments, suggesting that medication cost alone was not responsible for the racial/ethnic disparities we observed. Furthermore, this study extends the data demonstrating that not only are white patients with AF more likely to initiate OACs, racial and ethnic minorities are both not as likely to initiate OAC, in particular more effective DOACs, despite their availability on the VA formulary. So where do we go from here? In February 2021, our team received funding from VA HSR&D through a Career Development Award entitled, “Access, Quality, and Equity of Anticoagulation in Veterans with Atrial Fibrillation.” This three-aimed study seeks to 1) characterize the association between race, ethnicity, and oral anticoagulant initiation in Veterans with AF; 2) examine stakeholder perceptions of the barriers to and facilitators of equitable oral anticoagulant initiation in Veterans with AF; and 3) design and pilot test an implementation strategy bundle to improve equitable oral anticoagulant initiation in Veterans with AF. Our goal is to use AF as an exemplary model disease through which we can understand and reduce treatment disparities across the VA health system and beyond. These steps can lead our health system closer to achieving pharmacoequity, a goal where all patients, regardless of race, class, or availability of resources, have access to the highest quality of treatment they need. References
|
|