
|
|
Research HighlightEmergency Care in the Community: An Emerging Priority Area for HSR&DKey Points
VA has a long history of partnering with the non-VA healthcare community to ensure Veterans receive timely access to emergency care when unscheduled acute care needs arise. In recent years, implementation of the Veterans Choice Program, and more recently, the MISSION Act, greatly increased opportunities for Veterans to receive care in the community, thereby substantially expanding VA’s role as a purchaser of care. During this time, VA also began offering a new urgent care (UC) benefit that allows eligible Veterans to receive UC from providers within VA’s community network, without prior authorization from VA. Concomitant changes in emergency care payment authorities, notification processes, and reimbursement rates have simplified the process of approving and paying for community emergency care. As a result of these collective changes, VA has experienced an unprecedented increase in demand for community-based acute care, and substantial pressure on its overall budget (see Figures 1, 2, and 3). Emergency care is now the single largest contributor to VA community care spending and is rising rapidly, as non-VA Emergency Department (ED) visit expenditures are up 46 percent since 2020.1 In response to these trends, VA launched the Care Optimization in the Emergency Department (CO-ED) initiative in the spring of 2021. CO-ED is a joint initiative between the Office of Integrated Veteran’s Care (IVC) (a merger of the former Office of Veterans Access to Care (OVAC) and Office of Community Care (OCC)), Emergency Medicine, VISN leaders, and other key program offices and subject matter experts in the field. One of the chief aims of CO-ED is to optimize VA processes and resources to execute more economical methods of value-based care that result in the right care, at the right place, at the right time for Veterans. To understand and prioritize research on emergency care for Veterans, HSR&D convened the State-of-the-Art Conference on VA Emergency Medicine (SAVE) in 2022 with researchers, operational leaders, and stakeholders in attendance. In addition to the need for research for Veteran emergency care in general, attendees identified four specific high-priority focus areas, including emergency care in the community. The community care (CC) workgroup articulated the following priorities: (1) examining changes in patterns of use and costs in VA and CC as a result of recent policy and coverage changes (with an emphasis on modifiable factors); (2) understanding quality, safety, and Veteran experience differences between VA and CC settings; and (3) understanding follow-up needs among Veterans who have received CC emergency care (or UC), and how well those needs are being coordinated, communicated, and met. A more detailed description of these priorities is available here. Understanding the Key Drivers of Community Care ED Use and Costs: The Acute Care and Emergencies (ACE) Team*We assembled a team with expertise in emergency care, quality measurement, policy and economic analysis, and qualitative methods to better understand Veteran use of emergency care in and outside VA. The ACE team partnered with the CO-ED team to conduct analyses that will elucidate the key drivers of CC ED utilization and costs. Our preliminary findings include the following:
(Veterans with four or more ED visits in one year) has doubled, but this group only accounts for 21 percent of all CC ED visits and 19 percent of CC ED costs.
The ACE team has also interviewed Veterans to better understand their setting choice (VA vs. community) preferences, satisfaction with ED care provided in the community, and experiences navigating community emergency care. Findings included the following:
In another analysis of the MISSION Act urgent care benefit, the ACE team found the following:3
Future work by the ACE team will examine predictors of VA and CC ED use, and factors that can help identify differences in the quality of ED care received by Veterans in the community versus VA. Accessing emergency care is challenging for Veterans who use VA for healthcare, in part because the VA ED footprint is limited. As an increasing number of Veterans are treated in community EDs, it is vitally important that we better understand the access, quality, safety, and cost implications associated with this shift. The confluence of operational partner needs and HSR&D priorities makes this an ideal time for interested VA researchers to engage in this high priority area. *ACE Team: Anita Vashi MD, MPH, MHS; Tracy Urech, MPH; Diem Tran, PhD; Liam Rose, PhD; Andrea Nevedal, PhD; Steven Asch MD, MPH; Todd Wagner, PhD; Derek Boothroyd, PhD; Aaron Dalton, MA, MSW; Winnie Wu, MPH; Lena Schoemaker, MS 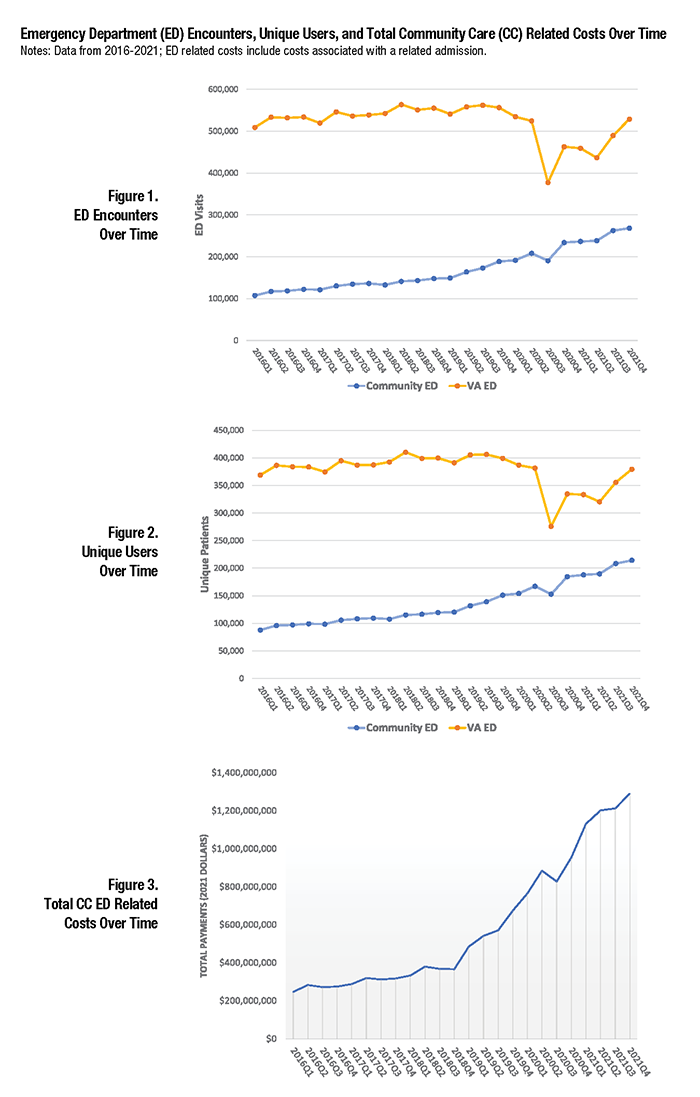
References
|
|