
|
|

Research HighlightStudy Points to Racial and Ethnic Disparities in Bereaved Family Reports of Veterans' Care Near the End of LifeThe demographics of the U.S. Veteran population are rapidly shifting. Currently, racial and ethnic minority Veterans comprise about 25 percent of the total Veteran population; however, this percentage is expected to approach 40 percent by 2045.1 The Veteran population is also aging, with an expected surge of Vietnam-era Veteran deaths over the next 10 years. Given these changes, ensuring the delivery of culturally sensitive care to seriously ill Veterans and those near end-of-life (EOL) is imperative. Although VA has made significant efforts in identifying and eliminating health disparities in a wide range of clinical areas over the past decade, very little research has focused on racial and ethnic differences in VA quality outcomes among seriously ill Veterans near EOL. Since 2012, the Veteran Experience Center has administered the Bereaved Family Survey (BFS) to the next-of-kin of all Veterans who die as an inpatient in VA Medical Centers (VAMCs) and Community Living Centers nationally. The BFS collects information about the Veteran and family experience of care received during the last month of life. Sixteen Likert-type items are included on the survey that relate to specific aspects of care, such as communication with providers, alignment of care with preferences, emotional and spiritual support, receipt of death benefit information, as well as items related to pain and post-traumatic stress symptom management. A global item included on the survey – the BFS Performance Measure (BFS-PM) – evaluates the overall quality of care received during the last month of life. The BFS-PM, a National Quality Forum-endorsed measure, is used by VA to monitor the quality of EOL care provided in VA facilities. Two open- ended items on the BFS ask families to share any additional observations about the Veteran’s care and suggestions for improvement. Using five years of national BFS data linked with medical records, our team conducted one of the largest examinations of race, ethnicity, and the quality of EOL care provided in VA inpatient settings.2 In our review of over 94,000 Veteran records, we found no statistically significant differences by race or ethnicity for the receipt of a palliative care consult and the occurrence of death in an inpatient hospice unit – two care processes that are associated with more favorable family ratings of overall EOL care. Figure 1 shows selected BFS outcomes from the study by race and ethnicity. Families of black and Hispanic Veterans were significantly less likely than families of white Veterans to report that the care received during the last month of life was excellent. Lower scores for racial and ethnic minorities were also noted among other important aspects of EOL care, including the meeting of personal care needs, management of post-traumatic stress symptoms, and the receipt of enough spiritual and emotional support. The results suggest that despite similar usage of services associated with high-quality EOL care across race and ethnicity, perceptions of the quality of that care by family members of minority Veterans are generally less favorable than those who are non-Hispanic white. This work illuminated the critical importance of family perceptions in evaluations of equity and quality of EOL care and that more research is needed to understand why racial and ethnic differences in perceptions of quality EOL care exist. Studies conducted in non-VA settings have found that racial and ethnic minorities are more likely to prefer life-prolonging, intense treatments near EOL and may be more likely to experience potentially burdensome transitions (i.e., multiple hospital admissions in the last months of life or a final hospitalization with a short length of stay) as compared to non-minorities. These care patterns may contribute to overall dissatisfaction with care when rated by patients and their families. Our prior work has also demonstrated that organizational factors, specifically related to nursing care, are also important to patient outcomes, including quality of EOL care.3 Organizational aspects of nursing care, including staffing levels and work environment conditions, directly impact a nurse’s ability to provide optimal patient care. Nursing may be an especially important area of focus in the study of EOL quality disparities as nurses are often the care providers who spend the most time with patients and their families, and are in a position to learn and communicate the Veteran’s care preferences to other members of the healthcare team. Using a mixed-methods approach, an HSR&D funded study is currently underway that seeks to identify whether patient-level factors (i.e., aggressive care/life-sustaining treatments and potentially burdensome transitions), and VAMC-level factors related to nursing care explain the observed racial and ethnic differences in BFS outcomes. Using several merged VA data sources from FY2011-2015, including the VA Nursing Outcomes Database (VANOD) and Corporate Data Warehouse (CDW), the sample includes nearly all inpatient deaths and their associated BFS responses, representing 142 VA Medical Centers nationally. In addition, we also aim to understand the needs and preferences of minority Veterans and their families at the EOL through a qualitative analysis of BFS data. The results will significantly advance our understanding of the needs and preferences of seriously ill minority patients near EOL and their families, and will provide actionable guidance to VA clinicians and administrators to move towards the elimination of these disparities. 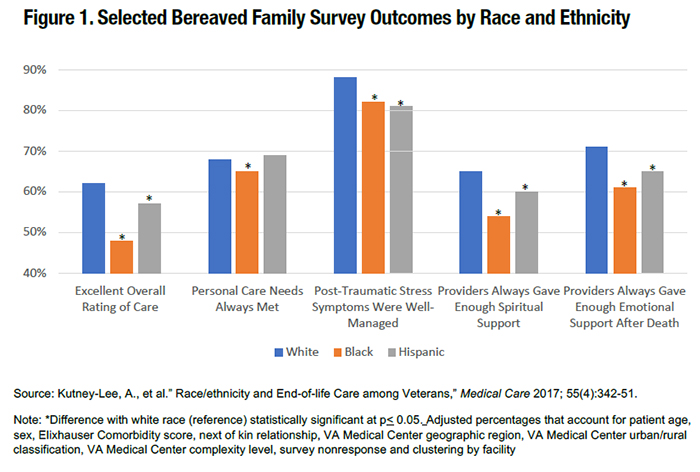
References
|
|