
|
|
Research HighlightWhole Health Improves Veterans' Experience and Patient-Reported OutcomesThe VA Office of Patient Centered Care and Cultural Transformation (OPCC&CT) has been promoting patient-centered care through the implementation of the Whole Health System of Care. OPCC&CT defines Whole Health as an “approach to healthcare that empowers and equips people to take charge of their health and well-being and live their life to the fullest.” The goal is to transform the organization and culture of care to a system which starts with understanding the Veteran’s life mission, aspiration, and purpose (i.e., what matters most to the Veteran) and then provides care to improve Veterans’ overall health and well-being. Whole Health integrates peer-led explorations of Veterans’ mission, aspiration, and purpose, personalized health planning, and use of Whole Health coaches and well-being classes, with both allopathic, and complementary and integrative clinical care that focuses on Veterans’ goals and priorities. The Whole Health System of Care is comprised of three major components: 1) Whole Health Pathway – in which Veterans are introduced, often by peers, to the concepts of Whole Health, explore their mission, aspiration, and purpose, and develop a personal health plan; 2) Whole Health Clinical Care – in which Veterans receive care from providers trained to provide Whole Health care, focusing on Veterans’ personal health plans and goals aligned with their mission, aspiration, and purpose as a foundation for treatment recommendations; and 3) well-being programs in which Veterans participate in complementary and integrative health services, health coaching and support, and other self-care and skill-building groups to support them in managing their own health. In October 2017, as part of VA’s response to mandates in the Comprehensive Addiction and Recovery Act,1 Directors of each of VA’s 18 Veterans Integrated Service Networks selected one facility to participate in piloting the Whole Health System of Care (WHS). The Center for Evaluating Patient-centered Care (EPCC), a QUERI Partnered Evaluation Initiative, conducted a comprehensive evaluation of the implementation of WHS and its impact on Veterans with chronic pain. We conducted a longitudinal survey (baseline, 6 months, and 12 months) of Veterans receiving care at the 18 flagship sites, to assess a range of Veteran-reported outcomes believed to be impacted by the WHS: 1) perceptions of care; 2) engagement in care; 3) sense of life meaning and purpose; 4) health and well-being (functional status, perceived stress); and 5) pain intensity and its impact. While our evaluation is ongoing, early analysis of change in patient reported outcomes at six months for 3,266 respondents shows meaningful positive effect sizes in several areas. Comparing Veterans who used WHS services with those who did not, Veterans who used WHS services demonstrated greater improvements in experience of care with their primary care providers, and in patient-reported health and well-being outcomes. Findings were particularly strong among Veterans who were comprehensive WHS users, defined as having at least eight visits, including both core WH services (such as WH classes or WH coaching) and Complementary and Integrative Health services. Veterans who used WH services also reported positive experiences with their care. Those Veterans who used WHS services reported greater improvements in quality of healthcare interactions with VA providers and improved satisfaction with VA care compared to those who did not use WHS services. The largest improvements occurred in the response to two questions regarding Veterans’ personal health goals, indicating that Veterans who used WHS services more frequently discuss and get help with their personal health goals from providers, compared to non-users. Our preliminary findings support the inspiring impacts that Whole Health Flagship Leaders are seeing and hearing about every day. During qualitative interviews about implementing WHS at the flagship sites, a WH leader told this story of one Veteran’s experience with WH: We recently worked with a Veteran – he’s a retired colonel. Perfect example of what you want. He came to us with chronic pain, had struggled with it for quite some time. Started using acupuncture and chiropractic care, kind of the more passive modalities – someone doing something to you. Then he started doing some of our integrative pain academy…From there he started doing yoga and tai chi at VA. Then he started doing yoga in his community at his gym. And then he heard about a swim class at the gym, and now he’s swimming regularly at his gym! Coming to the VA for a couple of things but essentially is doing so well that he doesn’t really need us anymore! – (Site F, Whole Health Clinical Director) Another WH leader reflected on the stories she had heard from Veterans: When I think about what we are doing and the idea of “Caring for him who has borne the battle” … our Veterans deal with more than any other population – PTSD, chronic pain, anxiety, depression, suicide. The kinds of things that Whole Health approaches have to offer, just the way that it’s operationalized is what our Veterans need and haven’t gotten… I think of all the individual stories I’ve seen and heard of just truly transformed lives. People who felt like they’ve gotten their lives back. Those are the things to me that say we need to stay on this path. – (Site R, Whole Health Clinical Director) We are planning future qualitative interviews with Veterans to further uncover how and why WH works for them. Complete analysis of our full cohort will also enhance our understanding of the extent to which WH impacts Veterans’ health and well-being. Health services researchers need to take advantage of VA’s ongoing natural experiment of VA’s WHS implementation in order to learn how and for whom different components of the WHS work best.2 Creating a system of care that is truly patient-centered, focused on providing care that is aligned with each individual Veteran’s goals, is the highest priority. As the Veteran consultant for EPCC, Rodger Kingston, said upon hearing the outcomes of this evaluation “one of the best things [about Whole Health] is what it does to your state of mind.” Staying on the Whole Health path may truly transform Veterans’ healthcare and more importantly, Veterans’ lives. *Dr. Steven Zeliadt, Dr. Justeen Hyde, and investigators at Bedford/Boston, Seattle and Los Angeles COINs. 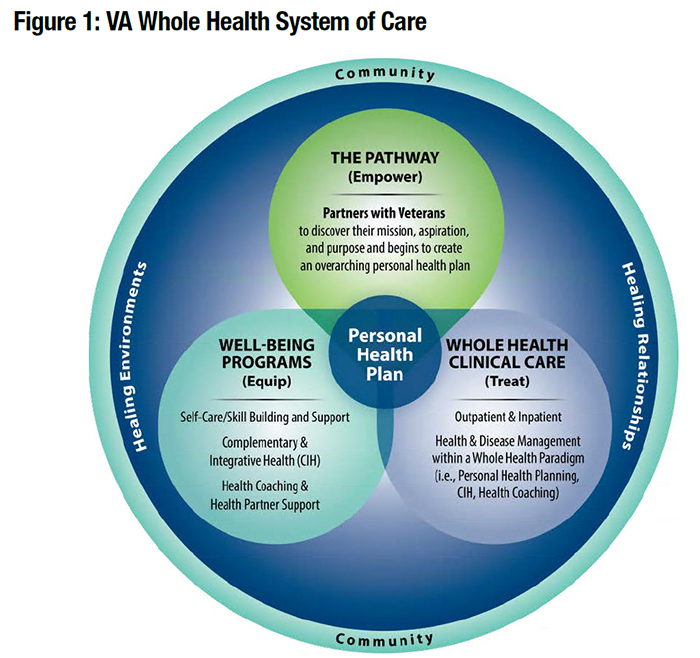
References
|
|