
|
|
Research HighlightData-Driven Insights to Inform Strategic Recruitment and Retention of VA Primary Care PhysiciansKey Points
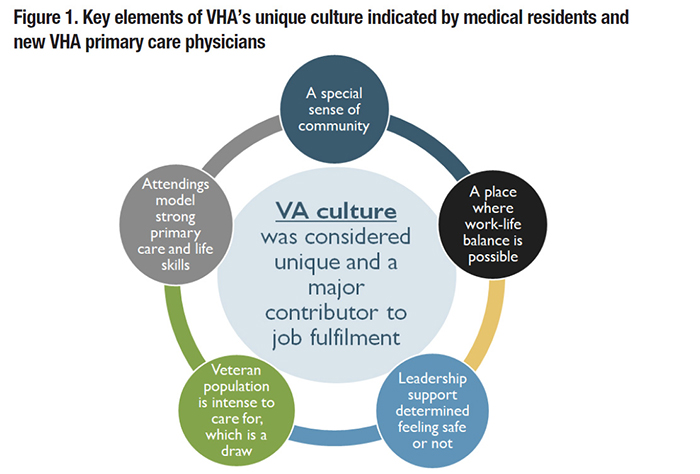
Maintaining a fully staffed and highly functioning Veterans Health Administration (VHA) workforce is one element of VHA’s promise of delivering high quality care to Veterans. However, some VHA facilities have faced staffing challenges, with 47,310 staff vacancies reported in public VA Mission Act Section 505 data as of the fourth quarter of 2021.1 A recent Inspector General report found 90 percent of VHA facilities had a “severe shortage” in at least one physician specialty.2 The ability to maintain a fully staffed workforce depends, in part, on the ability to successfully recruit and retain medical staff. However, little work has been done to inform strategic approaches to help stakeholders with these efforts. Such information is particularly timely given the current state of the labor market and the substantial hiring challenges within the healthcare sector. This FORUM article presents findings from an HSR&D Merit Review Study titled “Identifying Value Driven Approaches to Strengthening the VA Primary Physician Workforce.” We focus on issues of recruitment and retention in primary care physicians because primary care functions as the centerpiece for managing and coordinating care for Veterans within the Patient Aligned Care Team (PACT) medical home model. An overall goal of our study is to generate data-driven insights that cut across VA service lines and occupations. The issue of strategic recruitment of primary care physicians has been scarcely examined but offers substantial potential as VHA is the largest provider of medical training in the United States. Supporting positive experiences in VHA during training and reinforcing the desirable aspects of VHA employment may serve as a catalyst to motivate medical residents to pursue long-term careers in VHA. In partnership with the Office of Academic Affiliations, we conducted semi-structured phone interviews with 24 internal medicine residents and 30 newly hired primary care physicians to assess their training and employment experiences. For residents, we asked open-ended questions and follow-up probes about their experiences training in VHA and desirability of permanent employment in VHA. For newly hired primary care physicians, we asked about their experiences working in VHA primary care and why they chose VHA for employment. Qualitative content analysis revealed three core themes:
Overall, we found that alignment with VHA’s patient-centered mission and community-based culture served important roles in job satisfaction despite administrative and bureaucratic challenges. Future recruitment efforts targeting physicians based on these factors may yield the most success in bolstering the primary care physician workforce. To explore primary care physician retention, our study team analyzed individual- and clinic-level determinants of physician turnover. We developed a database of 6,631 primary care physicians practicing at VHA facilities nationally from 2012 through 2016. This database included characteristics constructed from VA’s data sources, including the Corporate Data Warehouse (CDW) and Personnel Accounting Integrated Data (PAID). Of particular interest were seven composite measures within the PACT Implementation Progress Index (PI2), which capture the degree to which primary care clinics had integrated core elements of the Patient-Centered Medical Home model.3 Applying discrete hazard models, we found that physicians employed in clinics that ranked higher in delivering accessible care were at lower risk of turnover. Two items in the “access composite” help explain this finding:
Other notable factors associated with lower turnover included higher total compensation, urban location, and internal medicine specialty. Given the importance of primary care provider staffing, clear metrics are needed to communicate the degree to which a clinic is under or overstaffed. Following a VHA Primary Care directive, full-time primary care physicians and advanced practice providers (e.g., nurse practitioners, physician assistants) have a maximum panel size of 1,200 and 900 patients, respectively. By comparing the number of assigned primary care patients with the number of full-time equivalent (FTE) physicians, one can determine primary care provider staffing levels at the clinic level. Our team developed a “gap metric,” which calculates the ratio of theoretical maximum patient capacity to the number of assigned patients at 916 primary care clinics between 2017 and 2021. During this period, 72 percent of VHA clinics were not fully staffed for at least one month and 6 percent of clinics were understaffed for the full tracking period; only 22 percent of clinics were fully staffed the entire four years. On average, rural clinics were understaffed 21 percent of the period, compared to 14 percent of the period for rural clinics. Considering the current 6,202 primary care provider FTE nationally, this represents a national staffing deficit of about 5 percent; it also identifies 10-15 percent of excess capacity that could potentially be re-deployed elsewhere to help with staffing shortages. Taken together, findings from our study reiterate the challenge of maintaining an adequate health workforce, particularly in rural VHA clinics. While VHA may not be a fit for all VHA trainees, survey data collected from our study indicate over 50 percent of internal medicine residents would consider VHA employment. Regardless, recruitment efforts should focus on these residents, particularly those who connect with VA’s unique culture. The findings further suggest that processes to improve access to care for Veterans have the added benefit of protecting against physician turnover. Furthermore, other clinical areas seeking to increase retention may benefit from adapting PACT-related processes to improve access to care as one strategy to support providers. References
|
|