
|
|
Research HighlightBurnout, COVID-19 Perceptions, and Inclusion, Diversity, Equity, and Authenticity (IDEA) amongst VHA EmployeesKey Points
Our lives have changed dramatically since the COVID-19 pandemic, both personally and professionally (Cho, 2020; Hupkau& Petrongolo, 2020). Most VA employees who can perform their work from home have continued to telework through 2021. However, not all VA jobs can be performed from home (e.g., treating patients), and not all VA employees can continue to put their own (and their family’s) health in danger by risking exposure to COVID-19 by working on campus or in person. Clearly, COVID-19 is an added stressor in the VA work environment. Using 2021 VA All Employee Survey (AES) data, this article describes employee attitudes and perceptions about burnout, COVID-19 related stress, and the relationship of these perceptions to inclusion, diversity, equity, and authenticity (IDEA). Burnout Perceptions of VHA EmployeesOverall, 2021 AES data show that few VHA employees (5 percent) reported the highest level of burnout. Because burnout is influenced by environmental factors, different occupation groups typically experience different burnout levels. Amongst the occupation groups (i.e., physicians, nurses, other clinical, administrative, and wage employees), wage employees reported the highest burnout scores. Administrative personnel, nursing staff, and other clinical staff reported similar burnout levels to one another, which were all higher than physicians. Among physicians, primary care physicians reported the highest average burnout score, followed by psychiatrists. Level one nurses reported the highest burnout across all types of nursing. Among other clinical staff, pharmacists and psychologists reported the highest burnout. Clinical schedulers reported the highest burnout among administrative personnel. Among wage employees, food-related occupations (e.g., canteen workers, cooks) reported higher burnout than other types of wage employees. Multiracial and Native American employees reported the highest average burnout score, notably higher than White and Asian employees. Native American employees reported the highest burnout within physicians, nurses, administrative, and other clinical occupations; multi-racial employees reported the highest burnout among wage employees. Women reported slightly higher burnout levels than men. The burnout gap between women and men was largest for physicians, other clinical occupations, and in wage jobs. COVID-19 Perceptions of VHA EmployeesOverall, VHA employees were satisfied with VA’s response to the COVID-19 pandemic. By occupation, wage employees were consistently less satisfied with the COVID- 19 response (i.e., having the skills to help coworkers, supervisor’s role preparation, and trusting COVID-19 related information from senior leadership). That is, wage employees expressed less satisfaction with the messaging from leadership around COVID-19. Overall, around 56 percent of VHA employees said that COVID-19 had added at least a moderate amount of stress, and about 23 percent said it had added high or an extreme amount of stress. Of those feeling high and extreme stress, staffing/coverage needs were identified as the greatest source of stress. The COVID-19 support most requested by VHA employees included improved staffing and coverage, and policy changes such as leave usage. This pattern appeared consistent for administrative personnel, nursing, and other clinical. Wage employees also voiced a need for pandemic response plan communication a need that aligns with their expressed lack of trust in the information provided by senior leadership. Physicians were the only occupation group to request logistical support (i.e., supplies, space) as a top priority. COVID-19 barriers to work identified most frequently by VHA employees included challenges with personal mental health (15 percent), other barriers (10 percent), and challenges with personal illness (9 percent). This pattern held true for administrative personnel, nurses, and wage employees. Other clinical staff and physicians identified access to childcare and technical abilities needed to operate virtual systems (e.g., Skype) as additional barriers. AES Vaccination DataBy June 2021, 78 percent of VA employees reported having received the COVID-19 vaccine. Vaccination rates varied widely among employees based upon their occupation. VA physicians reported the highest and quickest rate of vaccinations, where 90 percent of VA physicians received the vaccine by March 2021. Only 4 percent of physicians had not received the vaccine by June 2021. Occupations with the lowest reported vaccination rates included wage employees (27 percent), administrative employees (22 percent), and nursing staff (18 percent). As a group, wage employees had the lowest vaccination rate (27 percent) and a high percentage indicated that their position did not enable them to telework (76 percent). In June 2021, 18 percent of VHA employees indicated they would seek medical (8 percent) or other (10 percent) vaccine exemptions. Wage employees, administrative personnel, and nursing staff were most likely to state they would resign if VA mandated the COVID-19 vaccine for employees. Inclusion, Diversity, Equity, and Authenticity (IDEA) across VHA Overall, 12 percent of all VHA employees reported experiencing discrimination within their workgroup on the 2021 AES. Black (16 percent), Multiracial (18 percent), Native American/Alaskan (19 percent), and Native Hawaiian/Islander (17 percent) employees reported more discrimination than White employees (10 percent). These employees make up more than a quarter of VHA employees. Employees with disability (20 percent of VHA employees) had worse experiences than those without disability, reporting more discrimination, less inclusivity, less authenticity, and less opportunity. Women (64 percent of employees) reported lower scores on their experiences of inclusivity and opportunity than did men. Across sexual orientation identities, bisexual and other employees had worse experiences than straight employees across all IDEA scores. Employees who identified as gay or lesbian reported more discrimination and lower authenticity scores than straight employees. Employees who identified as transgender (approximately 0.5 percent) reported the worst experiences across all IDEA scores of any demographic measured by AES. That is, transgender employees experienced the highest rates of discrimination (30 percent) and had the lowest scores (i.e., more than half a point lower) of any demographic category for inclusivity, authenticity, and opportunity. Note that 43 percent of transgender employees are Veterans themselves and have slightly better experiences than non-Veteran transgender employees. In summary, few VHA employees reported high levels of burnout and wage employees reported the most burnout of any occupation group. Employees are satisfied with the VA COVID-19 response but reported improved staffing as the most common COVID-19 need. Twelve percent of VHA employees reported experiencing discrimination, indicating that we can all help make VHA the most inclusive environment possible. 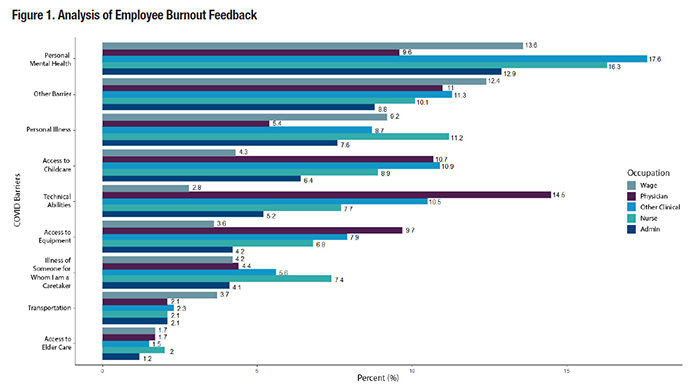
References
|
|