 |
Improving Quality and Safety of Care for Veterans with Chronic Obstructive Pulmonary DiseaseHSR&D’s monthly publication Veterans’ Perspectives highlights research conducted by QUERI investigators, showcasing the importance of research for Veterans – and the importance of Veterans for research. In the January 2019 Issue:The Quality and Safety National QUERI Program |
IntroductionSafety and Quality QUERI ProgramSafety and Quality QUERI works with operational partners – VA’s Pharmacy Benefits Management Service (PBM), Office of Specialty Care Services (SCS), and Geriatrics and Extended Care (GEC) – to identify and prioritize diagnostics and therapeutics that are ineffective, contraindicated, or of low value to Veterans, as they continue to enhance the science of de-implementation.Veterans with chronic obstructive pulmonary disease (COPD) can experience trouble breathing, and are often put on medications to help alleviate problems with breathing. For example, an inhaled corticosteroid can be helpful if they have frequent or severe breathing difficulties. However, for Veterans with mild or moderate and infrequent breathing difficulties, there are other medications that are as (and even more) effective, and an inhaled corticosteroid increases a patient’s risk of severe pneumonia, a potentially life-threatening illness. On average, for every 62 patients on an inhaled corticosteroid, 1 will get pneumonia. Unfortunately, with rapidly changing guidelines for many chronic conditions, it is challenging to stay up to date on every disease process and treatment. As a result, only about half of primary care providers surveyed were aware of the risks posed by an inhaled corticosteroid. Pulmonary specialists, who might recommend against use of an inhaled corticosteroid, are engaged only when the Veteran is having worsening breathing problems. This can lead to a missed opportunity to reduce a potentially harmful medication. 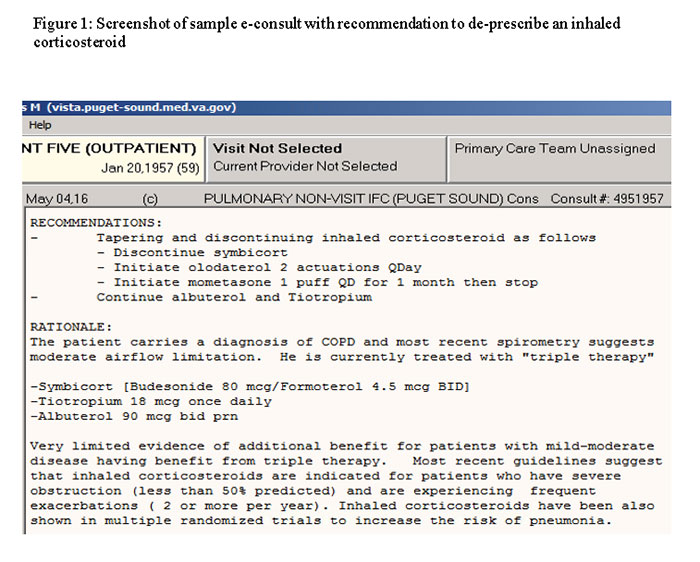
46% Percentage of primary care providers who report they were unaware inhaled corticosteroid is associated with a higher risk of pneumonia.Flipping the pulmonary-specialty consult on its headThe Quality and Safety National QUERI Program decided to try flipping this consultation model, and is testing a specialist-initiated consultation. In this model, a pulmonary specialty team uses the electronic health record to routinely scan for Veterans with COPD on an inhaled corticosteroid with an upcoming appointment. The pulmonary specialty team reviews the Veteran’s chart and determines if there is a reason the patient should be on an inhaled corticosteroid (e.g., perhaps they also have asthma or frequent COPD exacerbations). If there doesn’t appear to be a reason for the inhaled corticosteroid, the team enters a note with a recommendation to make a change, for example tapering and discontinuing the inhaled corticosteroid. They might make other recommendations, including getting a pulmonary function test to make sure the Veteran really has COPD and isn’t short of breath for another reason, e.g., heart failure. Figure 1 is an example of what an electronic consult note looks like. The primary care provider gets the note 1-2 days ahead of the Veteran’s visit and decides what to do. The note explains why the pulmonary team is recommending the changes, and includes links to guidelines and published research in case the primary care providers are interested in more information. What primary care providers told QUERI researchers before starting electronic consultations"...But deep down there's a little hesitation that if someone is doing well, "why rock the boat?" Primary care provider before starting the electronic pulmonary consults. There was still the question of how Veterans would feel when their provider went to take them off an inhaled corticosteroid. One of the concerns in the research literature about efforts to reduce unnecessary care, in general, is how it will affect patients’ trust in their doctors, and fear that they’re receiving poor quality care. Safety and Quality QUERI researchers talked with both Veterans and their primary care providers, and conducted a survey of all providers after they had received electronic consults to find out how they responded. When researchers spoke with providers before starting the electronic consults, several said their patients thought the inhaled corticosteroid helped them, and had misgivings about making a change in the absence of a specific problem. One provider said, “Generally, on one hand I’d like to say to someone who’s on medication they don’t need, you should try to stop it. But deep down there’s a little hesitation that if someone is doing well, why rock the boat This misgiving about not rocking the boat was compounded by a couple of dynamics. One was the aforementioned lack of awareness about the risks associated with inhaled corticosteroid prescriptions. Because inhaled corticosteroid is seen as fairly benign, there’s no counterweight to clinical inertia or patients’ feelings that the inhaled corticosteroid helps. One provider said of the inhalers, “They’re obviously not cheap necessarily, but they also do have side effects. But they’re not terrible… if the patient is really insisting that they’re helpful, I would tend to continue them.” Another compounding factor was the involvement of other providers, particularly when another provider put the Veteran on the inhaler in the first instance. One provider explained, “If someone came in on inhaled corticosteroid [inhaled corticosteroids] or if someone sees a pulmonary provider who prescribed it, I would probably be reluctant to stop it. But, most likely I would not initiate it.” When we surveyed providers about this, 39% reported they were unlikely to take patients off an inhaled corticosteroid prescribed by another provider. What happens when Veterans are taken off a corticosteroid inhaler?"...a security blanket...just to have it here in case..." Veteran whose primary care provider took him off an inhaled corticosteroid. QUERI investigators began the proactive pulmonary electronic consults in September 2016, and are performing them at 13 VA community based outpatient clinics in New England and the Pacific Northwest. They are interviewing primary care providers who receive at least two pulmonary consults, and interviewing Veterans who had been seen at a visit where an electronic consult had been made recommending taking the Veteran off an inhaled corticosteroid. The primary care providers researchers have spoken with have generally reported patients being receptive to the change. One provider reported, “If they don’t need the medication, there’s not much point in prescribing something that’s only going to do them harm…most of my patients were very receptive to that.” Some providers did report that Veterans felt the inhaled corticosteroid helped: “…they feel like something is working very well so they don’t want to change it, even though they may not have the exact indication for it.” And at least one provider put their patient back on an inhaled corticosteroid because the patient wanted it. 90% Percentage of primary care providers who report their patients were receptive to being taken off an inhaled corticosteroid.Veterans generally deferred to their primary care providers: “I just do what the doctor says so they don’t yell at me” or “Whatever the doctors think, because they have more schooling than I’ve got…” At the same time, one patient described inhaled corticosteroid as “a security blanket” that they wanted to keep it “…just to have it here in case…”. QUERI researchers surveyed all providers at the clinics to find out how many had proposed discontinuing or reducing an inhaled corticosteroid prescription for a patient in the past six months, and 54% reported they had. Of this group, 90% reported that their patients responded somewhat or very receptively, and 80% discontinued the inhaled corticosteroid or switched it to another medication. These providers have also generally been appreciative for the help. One provider wrote, “Overall it's been an effective, helpful program for me. More things like this for us overworked primary care providers!” What’s next?QUERI researchers are talking with more Veterans who have had an inhaled corticosteroid de-prescribed, and with primary care providers to make sure they get everyone’s perspective—both about the issue of low-value inhaled corticosteroid prescriptions, and about the proactive specialty electronic consult. Further, researchers are studying the provider survey data to see whether providers’ awareness has increased about the risks associated with inhaled corticosteroid prescriptions, and alternative medications to use. In addition, they will analyze inhaled corticosteroid prescribing and de-prescribing practices between the providers who received the electronic consultations and a set of providers who did not, in order to understand if there was an effect on Veterans’ care. For more information about this QUERI project, please contact Barbara Majerczyk, MPH, at barbara.majerczyk@va.gov. |