
|
|
Research HighlightWhole Health for Employee Morale: Addressing Workforce NeedsKey Points
The VA Office of Patient-Centered Care and Cultural Transformation (OPCC&CT) launched with the goal of introducing whole health into clinical practice and transforming the approach to Veteran care from “what’s the matter with you” to “what matters to you.” Since that time, OPCC&CT’s priorities have evolved to include the goal of bringing the whole health experience to employees. VA’s efforts to improve employee well- being started in 2008 and have expanded to encourage VA employees across all medicalcenters to increase physical activity, improve nutrition, stress management, and pursue smoking cessation along with other health- focused programs. Initially, VA viewed the program as a benefit for employees to allow them the chance to live a healthier life. In the last few years, VA has also emphasized the alignment between whole health systems of care components and empowering employees in areas of self-care, health, and well-being. Offerings for employees include complementary and integrative health (CIH) practices (e.g., meditation, yoga), and self-care education classes (e.g., tobacco cessation, nutrition, stress management). Research has linked employee whole health practices to the development of greater resilience, the adoption of stress management skills, and better management of burnout and other negative workplace emotions. While systems-level features (e.g., social support, resources, job demands, and work-life integration) can influence burnout, employees who focus on engaging in self-care practices have reported a greater ability to manage these types of stressors at work. The COVID-19 pandemic led to increased efforts across VA facilities to support employee well-being by expanding their offering and support of Employee Whole Health (EWH).Facilities offered courses and materials through online mediums that allowed employees access to virtual sessions and expanded the variety and number of offerings. Popular session topics and activities have included mindfulness, building resilience, yoga, and Tai Chi. Managers also encouraged employees to participate and set specific performance goals involving EWH. A recent evaluation effort conducted by the Evaluating Patient-Centered Care (EPCC) QUERI Partnered Evaluation Initiative (Bedford, Mass.) in 2021 consisted of interviews with 27 members of EWH implementation teams across 10 VA medical centers about factors that facilitated or challenged implementation. Implementation teams identified a variety of these factors, including practices related to leadership commitment and engagement, systematic organizational efforts, communication with employees, champions, and staffing of the implementation team. Implementation teams also reported that dedicated time and recognition of EWH as a priority by middle managers, along with the culture of the medical center are critical for sustaining the EWH program. A key question resulting from these efforts is whether EWH has impacted workforce morale. Prior work involving the VA All Employee Survey (AES) over the last several years (2018– 2021) has examined clinician participation in delivering whole health care to Veterans and its association with personal experiences at work. Findings suggest that employees who were able to participate in training, discuss whole health concepts with coworkers, and deliver care to patients aligned with the whole health model reported more favorable ratings of their medical center as a best place to work, experienced greater work motivation, had lower intent to leave, and lower reported burnout rates. One reason why whole health may have influenced these ratings is that EWH can provide clinicians with greater flexibility in how they provide care and can encourage better and more personal connections with their patients. In fact, sites that reported greater whole health involvement also reported higher patient ratings of care. In 2021, the AES asked employees about participation in various EWH activities consisting of CIH and self-education courses. Employees who participated in more sessions reported lower rates of burnout and perceived their workplaces more positively, including their relationships with managers, supervisors, and their own levels of motivation (Figure 1). 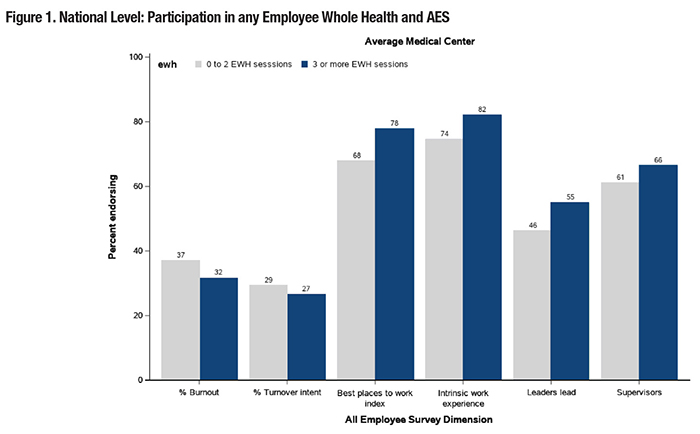
Another recent evaluation in 2021 by EPCC involved interviews of 31 employees about their participation in EWH activities, how they felt participation influenced work itself, as well as factors that facilitated participation. Employees indicated that convenience of activities, such as course offering times and virtual or recorded sessions, allowed for greater ease of participation during the day and offered a much-needed mental break from work. Other employees noted that after participating in an EWH activity, they had a better understanding of what it entails, and greater confidence and willingness to recommend similar activities to patients. Employees also noted the importance of supervisors and medical center directors who send clear and positive messages that support employees’ participation in EWH. In fact, a recent pilot study led by OPCC&CT has started to examine the effect of allowing 30 minutes per week of dedicated time for EWH. Further, those who participated in EWH activities reported feeling less stressed and reported that they felt a greater ability to deal with difficult situations on the job. One individual reported that mindfulness practices would better prepare her to engage in difficult conversations with family members of Veterans. To support EWH, clear VA policies and guidance would help encourage and support employees in taking time to participate in EWH activities. Such an effort may lead to a more refreshed and focused employee workforce, an important issue given the staff retention challenges that VA and other health care systems are currently experiencing. References
|
|