
|
|
Research HighlightImplementing Medication Treatment for Opioid Use Disorder in VA FacilitiesKey Points
Despite reductions in opioid prescribing, opioid use disorders (OUD) and overdose deaths among Veterans have continued to rise. Use of efficacious and cost-effective medications for the treatment of opioid use disorder (MOUD), including methadone, buprenorphine, and naltrexone, is associated with reduced opioid use and mortality. Historically, MOUD in VA has been prescribed through substance use disorder specialty care clinics and therefore has not reached Veterans who do not visit these clinics. To expand access to MOUD, VA’s Office of Mental Health and Suicide Prevention (OMHSP) launched the Stepped Care for Opioid Use Disorder Train-the-Trainer (SCOUTT) Initiative. SCOUTT aims to improve access to MOUD in primary care, pain management, and mental health clinics (hereafter Level-1 clinics) at 18 VA facilities nationwide in Phase 1, followed by an additional 18 facilities in Phase 2. Because methadone is available only in licensed opioid treatment programs, SCOUTT is focused on increasing prescribing of buprenorphine and injectable naltrexone. A Stepped Care, Population-Based ApproachSCOUTT uses a stepped care, population- based approach that promotes screening, assessment, and management of health conditions with the most effective, yet least intensive, intervention first, stepping up intensity of care as needed. SCOUTT launched in August 2018, with an in-person two-day meeting to train implementation teams to deliver MOUD using two proven treatment models for OUD: medication management and collaborative care. Facility-based implementation teams are cross- disciplinary and include Veterans Integrated Service Networks (VISN) leaders and four to five providers representing clinic leadership, prescribers, medical staff, behavioral experts, and pharmacists. Implementation teams assist with the spread of MOUD treatment using a train-the-trainer model, in which team members receive training to deliver intervention content and then train others to do the same to spread the intervention. Two Health Services Research & Development (HSR&D) Partnered Evaluation Centers received funding to deliver implementation facilitation and to evaluate, quantitatively and qualitatively, the success of the SCOUTT initiative. We summarize findings related to SCOUTT’s external facilitation approach and prescribers’ attitudes on prescribing MOUD in the initial year of SCOUTT implementation. SCOUTT employs an ongoing, external approach to implementation facilitation that includes conference calls with implementation teams to identify and address implementation barriers, monthly all-site conference calls to promote community-building, webinars to address gaps in providers’ knowledge, and expert consultation and/or site visits. External facilitation strategies were designed to address barriers commonly reported by clinicians, including stigma and/or discomfort around providing MOUD treatment, concerns about being overwhelmed by requests to prescribe buprenorphine, and gaps in providers’ knowledge about OUD and its treatment. While prior studies have examined primary care physicians’ attitudes regarding MOUD, few have been conducted in VA outpatient settings, included non-MD prescribers or prescribers from a variety of settings, or examined changes in attitudes over time. To inform ongoing external facilitation and evaluate SCOUTT implementation, we conducted a longitudinal survey during the first year of the initiative to understand factors associated with successful implementation, including providers’ attitudes about MOUD–assessed by the Drug and Drug Problems Perceptions Questionnaire (DDPPQ) subscales–and barriers and facilitators to delivering MOUD in non-traditional settings. We hypothesized that providers’ perceptions of MOUD and the feasibility of delivering MOUD care would improve over time. All prescribers, MDs, and ARNPs, on the implementation teams were eligible to participate. We summarized responses and compared them using descriptive statistics. We used regression models adjusted for gender and clustered on facility to compare changes in subscale scores over time. SCOUTT Initiative ResultsSCOUTT implementation facilitators created a SharePoint site to serve as a resource hub, produced two monthly webinars to educate teams and address barriers, visited 10 SCOUTT facilities, and provided training in MOUD prescribing to over 100 clinicians. Overall, the SCOUTT Initiative was implemented in Level-1 clinics at 18 facilities to a varying degree of fidelity. By the end of 12 months, all 18 facilities increased MOUD prescribing. Implementation models vary widely and include medical management, collaborative care, and pharmacy-led and telemedicine approaches to expand care to VA Community-Based Outpatient Clinics (CBOCs). Implementation barriers included credentialing and privileging delays, knowledge gaps, and provider and patient-related stigma. Facilitators included clinician champions at facilities, leadership buy-in, existing robust SUD resources, and close coordination with OMHSP. Overall, 26 of 41 (63.4 percent) and 29 of 56 (51.8 percent) implementation team prescribers responded to the survey at baseline and follow-up, respectively. Approximately 65.4 percent of respondents at baseline and 81.4 percent at follow-up were 45 years or older; 57.7 percent at baseline and 42.9 percent at follow-up were women. Most prescribers were white and waivered to prescribe buprenorphine by the Drug Enforcement Administration. With regard to perspectives on MOUD prescribing, no differences were found between responses at baseline and follow-up. Most prescribers strongly agreed/agreed at baseline and follow-up that MOUD is evidence- based (96.2 percent vs. 88.9 percent), important (100.0 percent vs. 92.6 percent), and life-saving (100.0 percent vs. 92.6 percent), and can be integrated into their clinic’s procedures and workflow (80.8 percent vs. 85.2 percent). Few providers at baseline and follow-up reported MOUD as detracting from clinical responsibilities (19.2 percent vs. 14.8 percent) or risky in terms of patients diverting medications (7.7 percent vs. 7.1 percent). However, 38.5 percent of providers at baseline and 48.2 percent at follow-up reported that MOUD delivery is time-consuming. Prescriber attitudes assessed by the DDPPQ are shown in Figure 1, with lower scores indicating more favorable responses. Providers’ ratings of knowledge about OUD, comfort with asking patients about opioid misuse and related consequences, and job satisfaction did not improve over the initial year. Likewise, providers’ confidence in their professional ability to help patients with an OUD and perceived support from colleagues in addressing issues with providing OUD treatment showed no improvement at follow-up, relative to baseline. Although implementation team prescribers reported consistently favorable views about MOUD delivery over the initial year, strategies that improve knowledge of and comfort with treating OUD may be necessary to scale up MOUD in non-traditional VA settings. Phase 2 efforts will include regional conferences to train 18 additional implementation teams and consultation/mentoring with existing addiction treatment experts to address provider knowledge gaps. VA has prioritized expanding the reach of MOUD. Early results from the SCOUTT Initiative serve as a guide to address key barriers and implement system-wide changes to improve access to MOUD in non-traditional settings. 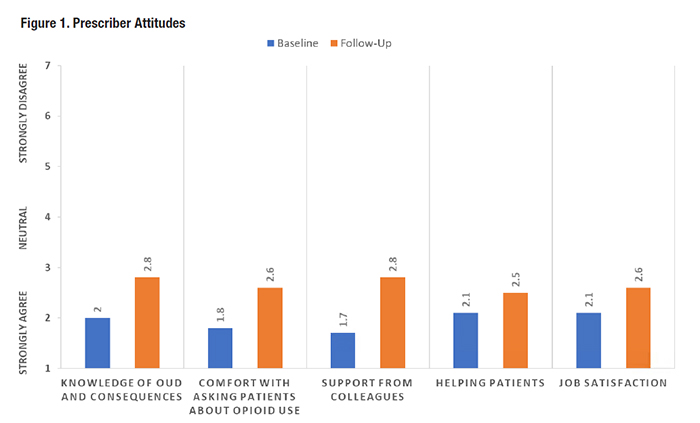
|
|