» Back to list of all Management Briefs

| Issue 186 | May 2021 | |
|
The report is a product of the VA/HSR Evidence Synthesis Program. Primary Care Engagement among Veterans with Experiences of Homelessness and Serious Mental Illness: An Evidence MapAdults with experiences of homelessness—those who have been homeless and those with housing insecurity— are more likely to suffer from chronic illness and early mortality compared with those who have not had experiences of homelessness. Adults who experience homelessness also have a higher mental health burden than the general population; about 20-25% of people who experience homelessness in the United States also have been diagnosed with serious mental illness (SMI). Both homelessness and mental illness negatively impact health and the receipt of healthcare and together those harms can be additive. Few interventions target both SMI and homelessness at the same time. For health systems to better meet the healthcare needs of this complex population, it is critical to learn about the types of interventions and strategies that have been developed and evaluated to better connect this marginalized patient population to primary care.
To this end, individuals with the National Center on Homelessness among Veterans requested a review summarizing the existing literature evaluating standardized, validated approaches to enhancing the engagement with primary care among individuals with homeless experience and SMI. Investigators with VA’s Evidence Synthesis Program (ESP) Center in Durham, NC conducted an evidence map of peer-reviewed literature that provides an overview of the intervention types and components that have been evaluated to improve engagement in primary care for individuals who have experienced homelessness and a diagnosis of SMI. Investigators searched MEDLINE®, EMBASE, and PsycINFO from database inception to May 15, 2020. They also hand-searched the bibliographies of previous systematic reviews related to primary care for patients with SMI – and those related to primary care for patients with experiences of homelessness for potential inclusion. After reviewing 4,650 unique citations, 191 were given a full-text review, with 22 articles describing 15 studies being selected for inclusion in this review. Summary of Findings Investigators did not find evidence of a standardized, validated approach to the promotion of primary care engagement for patients with homeless experience and SMI; rather they identified multiple programs describing various processes that attempted to link patients in the target population to primary care. Few programs in this review solely focused on linking the target population to primary care; rather, connecting patients to longitudinal medical care was often one of multiple intervention goals. Interventions were complex, particularly due to the use of various combinations of intervention strategies targeting multiple patient behaviors. The most common outcomes assessed to evaluate identified interventions included patient mental health status, substance use, criminal justice involvement, housing, and inpatient healthcare use. 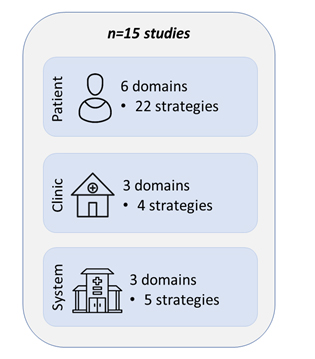
Additional findings from this review include:
Implications While some included studies were conducted in VA clinical settings, the majority were not. As such, caution should be used when generalizing these findings to a Veteran population. However, findings from this report will be relevant to VA as it seeks to continue the provision of high-quality, integrated clinical care to the Veteran population with housing insecurity and SMI through the development of pilot programs to serve the primary care needs of this vulnerable population. The results of this project also may be relevant to individuals, healthcare providers, and other agencies seeking to improve the health and quality of life for individuals with housing insecurity and SMI. Research Gaps/Future Research The current literature could be improved by rigorous study designs, standardized descriptions of intervention components, and a uniform and validated approach to measuring primary care engagement. Interventions should focus on maintaining primary care engagement over time as a critical focus for improving long-term health outcomes. Additionally, there is a need to validate outcome measures used in these studies to allow synthesis across future studies, particularly in relation to primary care engagement. Shepherd-Banigan M, Drake C, Dietch JR, Shapiro A, Alishahi Tabriz A, Van Voorhees E, Uthappa DM, Wang TW, Lusk J, Salcedo Rossitch S, Fulton J, Gordon AM, Ear B, Cantrell S, Gierisch JM, Williams JW, Goldstein KM. Primary Care Engagement Among Veterans with Housing Insecurity and Serious Mental Illness. Washington, DC: Evidence Synthesis Program, Health Services Research and Development Service, Office of Research and Development, Department of Veterans Affairs. VA ESP Project #09-010; 2021. To view the full report, go to vaww.hsrd.research.va.gov/publications/esp/pc-engagement.cfm (Intranet only, copy and paste URL into your browser if you have network access.) |
ESP is currently soliciting review topics from the broader VA community. Nominations will be accepted electronically using the online Topic Submission Form. If your topic is selected for a synthesis, you will be contacted by an ESP Center to refine the questions and determine a timeline for the report. This Management e-Brief is provided to inform you about recent HSR&D findings that may be of interest. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. If you have any questions or comments about this Brief, please email CIDER. The Center for Information Dissemination and Education Resources (CIDER) is a VA HSR&D Resource Center charged with disseminating important HSR&D findings and information to policy makers, managers, clinicians, and researchers working to improve the health and care of Veterans. |
|
|
This report is a product of VA/HSR&D's Evidence Synthesis Program (ESP), which was established to provide timely and accurate synthesis of targeted healthcare topics of particular importance to VA managers and policymakers –; and to disseminate these reports throughout VA. See all reports online. |
||