
|
|
CommentaryWhole Health: Focusing on What MattersThe Veterans Health Administration (VHA) has made a system-wide commitment to Whole Health, an approach to healthcare that empowers and equips Veterans to take charge of their health and well-being to live their lives to the fullest.1 This commitment is in response to a recognition that our country has built a healthcare system that is effective at treating many diseases – but does not focus enough on creating and supporting health and well-being, and does not do very well at addressing chronic pain, depression, loneliness, and the rising rate of suicide. Because of its focus on high-tech disease treatment, the United States spends far more than any other country on healthcare but ranks only 32nd in life expectancy.2 The COVID-19 pandemic has brought into focus even more clearly the need to create a health system that encourages self-care and builds well-being – rather than just a disease care system. At VA, we are expanding our understanding of what defines healthcare by developing a Whole Health System that provides both the highest quality disease-oriented care and that supports health and well-being creation. The Whole Health System also provides a tool to address what Don Berwick called the “moral determinants of health” by addressing the impact of structural and social determinants of health on Veteran well-being.3 The question “what’s the matter with you?” has generally been the guiding principle in our find-it/fix-it problem-based approach to healthcare. Whole Health shifts the focus to the question “what matters to you?” Whole Health places the Veteran at the center of the health creation team, and assumes that if everyone, including the Veteran, is aware of what they feel they need their health FOR, the plans they make as a team will have a much greater chance of becoming reality. This Whole Health approach has three key components: the Pathway, Well-being Programs, and Whole Health Clinical Care (see Figure 1). In the Pathway, Veterans meet with fellow Veterans who are trained as peer facilitators to discuss what matters to them in their lives. Together, they discuss the Veteran’s strengths and where they might need help to get to what matters. This peer-to-peer approach is critical in changing the conversation. The second component is the Well-being Program, where Veterans have access to covered evidence-based complementary and integrative health approaches like acupuncture and meditation, and learn new skills for self-management like yoga and Tai Chi. Veterans can also work with a Whole Health coach to make plans for how to address areas of their lives that need change. The third component is Whole Health Clinical Care, where Veterans continue to have their disease issues addressed and to access health promotion and prevention services. The key distinction is that these services are now delivered by clinical teams trained in how to ask about what matters to each Veteran, and how to place what matters at the center of the Veteran’s treatment and well-being plan. Evidence is mounting that the Whole Health approach is working for Veterans. Preliminary outcomes research on a three year Congressionally-mandated demonstration project at 18 “Whole Health flagship” sites around the country has shown this in several ways:4
This last finding – an increase on a validated measure of life meaning and purpose (the Life Engagement Test) – is especially important given the ongoing epidemic of Veteran suicide. Loss of purpose in life is a known risk factor for suicide. The Whole Health approach could have a significant role in helping address this epidemic by restoring a sense of purpose to Veterans who have lost it. Impact of the COVID-19 PandemicThe COVID-19 pandemic has led to some significant shifts in the Whole Health initiative. The intense workload and pressure experienced by VA staff during the pandemic has underscored the critical importance of caring for VHA staff. For several years we have been developing and supporting an employee Whole Health initiative that encourages VHA staff to adopt healthy behaviors, promotes self-care and well-being, reduces the incidence of preventable illness and injury, and that fosters a culture of employee engagement in order to ensure the best care and improved access for Veterans.5 Preliminary research from the Whole Health flagship sites shows that employees who reported involvement with this Whole Health initiative also reported their facility as a ‘best place to work’, and experienced lower voluntary turnover, lower burnout, and greater motivation. A VHA-wide expansion of the employee Whole Health initiative is a high priority in the next two years. A second major COVID-19 related shift was the rapid pivot in delivery of Whole Health from in-person settings to virtual. Total Tele-Whole Health visits grew from 12,058 visits by 3,679 unique Veterans in FY19 to 309,553 visits by 58,353 Veterans through the third quarter of FY21. VHA’s ability to deliver Whole Health services virtually was an unexpected development, as has been the extremely positive feedback from Veterans who are now able to access services like Whole Health coaching, Tai Chi, and meditation from the comfort of their homes. In response, many VISNs have built Whole Health services into their Clinical Resource Hubs in order to increase VISN-wide access. We anticipate continued rapid growth in the use of virtual technologies to deliver Whole Health services to Veterans. What’s Next for Whole Health?With the flagship demonstration project now completed, VHA will focus next on a national initiative to fully integrate the Whole Health approach into primary care and mental health settings across VHA over the next three years. This initiative is being driven by the Modernization Lane of Effort “Transforming Healthcare Delivery,” and is supported by the offices of Primary Care, Mental Health and Suicide Prevention, and Patient Centered Care & Cultural Transformation. The goal of this initiative is to ensure that every Veteran will walk away from each and every primary care or mental health visit feeling that the team knows what matters most to them in their life, and that the plan for treatment and well-being was informed by that knowledge. We are seeking to move beyond an exclusively disease and treatment-oriented model to one that is truly Veteran-centered. VHA is implementing this initiative at the 18 flagship sites, and will implement this approach at every VAMC over the course of two subsequent waves. Another important focus for the coming year is developing a strategy for measuring well-being as part of routine clinical care. Working with HSR&D colleagues, we are piloting a brief measure of well-being that can be incorporated into routine care to provide a tool to assess the impact of Whole Health and other interventions on overall Veteran well-being. As part of this effort, VHA co-sponsored a virtual meeting with colleagues from the National Center for Complementary and Integrative Health at NIH to begin discussions regarding the best strategies for measuring well-being in both clinical and research settings. Our belief is that developing and implementing simple ways for clinicians to ask about and measure well-being will help facilitate VHA’s “cultural transformation” towards Whole Health. 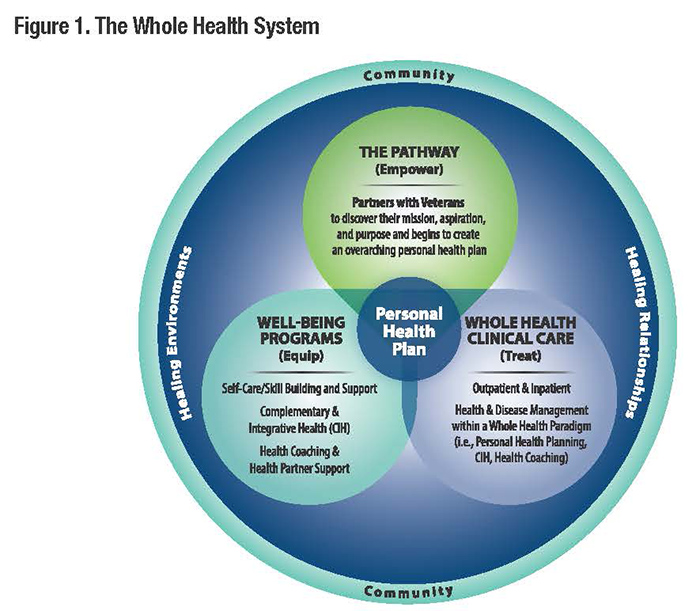
References
|
|
Next ❯