
|
|
Research HighlightWorking in COVID-19 Recovery: Importance of Alternative Evidence-Based Practice StrategiesKey Points
The COVID-19 public health emergency has disrupted access to face-to-face healthcare visits in unprecedented ways. Diagnostic and procedural services (e.g., radiology, interventional procedures, surgery) have been particularly susceptible to disruptions in care. This is primarily due to the challenge in shifting to virtual care for these services. Moreover, these services have frequently had to reduce their capacity as a result of staff redeployments, repurposing and reductions of space and equipment, and laborious protocols to screen and prevent transmission of the SARS-CoV-2 virus, which causes COVID-19.1 As a result, many procedural services in VA now have substantial backlogs that will likely take many months, if not years, to work down without strategic actions by VA to mitigate these backlogs. As part of an HSR&D-funded Rapid Response Project (RRP), we sought to understand whether the implementation of several evidence-based practice (EBP) strategies, which involve applying the best available research evidence in the appropriate clinical context, could improve access to gastrointestinal (GI) endoscopy. Our approach and findings can serve as a model for other clinical services during the COVID-19 system recovery phase. Opportunities to Improve Access in EndoscopyGI endoscopy is one of the most commonly performed ambulatory procedures in VA, with almost 400,000 procedures annually. Lower endoscopy (i.e., colonoscopy) is a mainstay of VHA’s colorectal cancer (CRC) prevention efforts, playing a role in both screening for cancer and surveillance to ensure that patients with previous CRC or pre-cancerous growths (i.e., polyps) do not have recurrence. Access to timely colonoscopy is essential because delays in diagnostic colonoscopy after an abnormal stool-based CRC screening test or in patients with previous high-risk polyps are associated with a higher risk of advanced CRC.2 Using discrete event simulation, an analytic method that models the behavior and performance of a real-life process, we evaluated the impact of two EBP strategies to reduce demand, and increase access, for colonoscopy during and after the first wave of the COVID-19 pandemic.
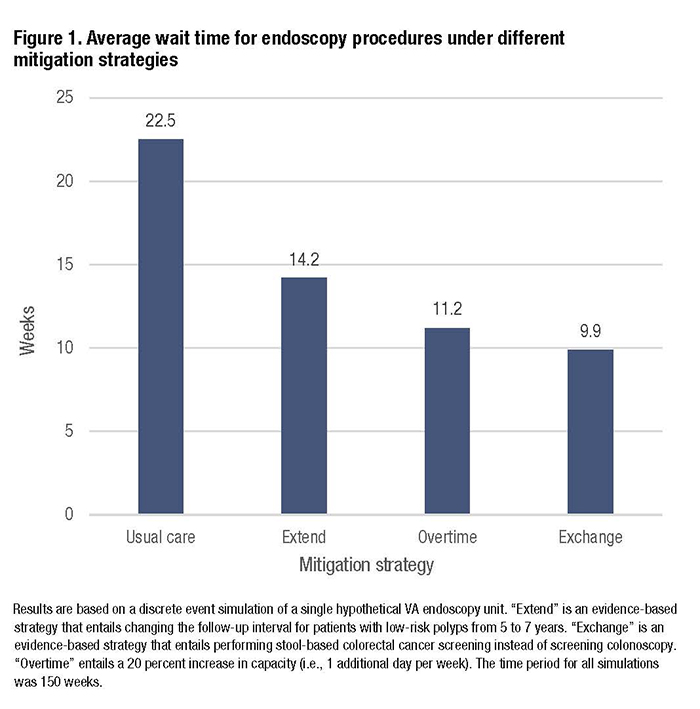
Results of Simulation ExerciseThe simulation model examined a hypothetical endoscopy unit that had a pre-COVID capacity of 110 procedures weekly, which is similar to many endoscopy units in VA. The unit was part of an integrated healthcare system without external referrals to community care. We made the following assumptions: 1) during the early pandemic, capacity was reduced to 5 percent of pre-COVID levels for 10 weeks; 2) capacity incrementally increased back to 100 percent by 30 weeks; 3) the number of referrals each week was 113; and 4) patients with the highest priority were always seen first, as recommended by VA GI National Program guidance, with all others joining a waiting line (i.e., queue). Using published VA data, referrals included (in descending order of priority) 23 percent for diagnostic colonoscopy, 28 percent for upper endoscopy, 10 percent for high-risk polyp surveillance, 17 percent for low-risk polyp surveillance, and 22 percent for screening colonoscopy. (The Extend strategy would be appropriate for low-risk polyp surveillance and the Exchange strategy would be appropriate for screening colonoscopy.) We compared the Extend and Exchange strategies to a scenario of 20 percent Overtime, which is equivalent to running the endoscopy unit one extra day per week, and to usual care. The model length was approximately three years (150 weeks). With usual care, the average wait time across all procedural indications was nearly six months, driven predominantly by wait times for screening colonoscopy, which exceeded one year; more than 3,000 patients remained in the queue at the end of the three-year period. The Exchange strategy reduced average wait times to the greatest degree (56 percent), followed by Overtime (50 percent) and Extend (37 percent; see Figure 1). Notably, with Exchange the wait time for screening colonoscopy was reduced to zero since all CRC screening was done using FIT, while with Overtime and Extend, average wait times for screening still exceeded 8 months. Both Exchange and Overtime reduced the queue to zero by three years, while over 1,000 patients remained in queue at three years with Extend. With all four strategies, nearly equivalent numbers of patients were seen for high-risk polyp surveillance, diagnostic colonoscopy and upper endoscopy, with similar wait times. ConclusionsThe COVID-19 pandemic has created an opportunity and urgency to maximize the value of care provided by VA, and in the process increase Veteran access. Simulation modeling can help VA clinical leaders evaluate and select evidence-based strategies to maximize access to critical services when it is limited by external or internal events. In the setting of gastrointestinal endoscopy, we found that wait times for the lowest priority endoscopy indications, particularly screening colonoscopy, will be unacceptable without the use of mitigation strategies, and that an evidence-based Exchange strategy has the greatest potential to mitigate the problem. Instead of simply working harder (e.g., employing overtime), working smarter (e.g., using FIT, instead of colonoscopy, for screening) may do more to improve access. References
|
|