
|
|
Research HighlightOpportunities to Improve Dementia Care for Aging VeteransKey Points
Increasingly, older adults are turning to emergency departments (EDs) to address healthcare needs. In fact, nearly 1 out of every 2 older U.S. adults (aged 65 and older) will visit the ED each year. Situated at the crossroads of outpatient and inpatient care, the ED is a safety net for lapses in care and an important partner in care coordination. With this growth in ED utilization comes the need to transform our current emergency care model to one that incorporates the unique needs of geriatric patients and reduces complications that commonly arise from ED encounters. VA Geriatric Emergency Departments: Leading the Way in Progressive Geriatrics CareVA is one of the largest integrated healthcare systems in the United States, with over a million ED visits made by older Veterans each year. More than 50 percent of all VA ED visits are made by older Veterans 65+ years in age, a figure that is substantially higher than the 15-16 percent of ED visits made by older patients in community EDs. Older Veterans utilizing VA EDs have higher rates of poor physical health, chronic diseases, complicated social needs, and a higher rate of repeat ED visits than non-Veteran older adults in the community. For these reasons, the integration of high quality, reliable geriatric emergency care processes will have a significant impact on the delivery of VA healthcare to older Veterans. In 2018, partnerships between VA’s National Emergency Medicine and Geriatrics and Extended Care Offices created a core team to disseminate age-friendly models of care to standardize use of best practices for geriatric emergency care screening of common geriatric syndromes. Currently, 72 of 110 VA EDs (65 percent) provide emergency care with geriatrics initiatives incorporated, and 63 of these EDs are recognized by the American College of Emergency Physicians (ACEP) for these achievements with Geriatric Emergency Department Accreditation (GEDA). In 2022, ACEP awarded VA its elite system GEDA status as the nation’s largest integrated healthcare system with GED accreditation. To demonstrate the spread of GED care practices in VA EDs, we compared rates of recommended geriatric syndrome screening in VAs with GED accreditation versus those without in an observational study from January 2018 to March 2022. 1 During the study period, there were over 4 million ED visits by Veterans 65+ years in age. Geriatric screens identifying older adults at risk for poor outcomes, delirium, and falls had the highest usage rates within VA GEDs. Veterans seen at GEDs with higher intensity accredited programs (Level 1) had 76-fold greater odds of having a GED screen than at lower level accredited GEDs (Level 3). VA ED Visits and Undiagnosed Dementia: An OpportunityPatients with cognitive impairment utilize health services and the ED more frequently and at greater cost than those without cognitive deficits. Diagnosis of dementia or mild cognitive impairment (MCI), however, is a complex and resource-intensive process, typically done in the outpatient setting. Approximately half of older adults with dementia are undiagnosed or unaware of their diagnosis. As such, screening older adults to identify those who would warrant formal testing is an important first step to direct limited resources in this area. While it is established that patients with diagnosed dementia have high rates of ED utilization, we also know that the ED sees a significant number of undiagnosed dementia patients, and this trend is anticipated to grow with the aging population. Additionally, serious events or acute illness can precede or even precipitate a diagnosis of dementia. Therefore, the ED may be an opportune setting to facilitate earlier recognition of dementia and MCI. We evaluated patterns of ED visits by older Veterans with dementia diagnoses in the months before and after their diagnoses. We identified many Veterans with a spike in ED visits in the 6 to 12 months prior to their first dementia diagnosis 2 detection that, in the past, was routinely missed in the outpatient and ED setting. The surge in ED visit encounters shown in Figure 1 highlights the ED visit as an opportunity to enhance recognition of those with missed or undiagnosed dementia; furthermore, the ED visit presents an opportunity to improve patient care transitions, increase safety to and from the ED, and facilitate referral processes for subsequent evaluation, diagnoses, and access to new treatments and trials. Augmenting Detection of Dementia in the EDAs older Veterans increasingly utilize EDs, there will be greater need to assess them for undiagnosed cognitive impairment and dementia and thus the opportunity to increase detection of these conditions. Reported rates of dementia for Veterans seen in VA EDs (14 percent) 3 are higher than those seen among patients in community EDs (7 percent). With their specific histories and combat exposures (including PTSD, depression, traumatic brain injury [TBI]), it is likely there may be even greater risk of cognitive impairment. Early evidence indicates TBI and exposure from repetitive improvised explosive device blast injuries on the battlefield are associated with a decline in cognitive function. We can leverage the innovation of AI and machine learning tools to augment emergency care recognition of those at risk for dementia. We have successfully tested and implemented dementia risk analysis using temporal event modeling in other large healthcare systems. Our goal is to bring these algorithms and techniques to the Veterans Health Administration.4 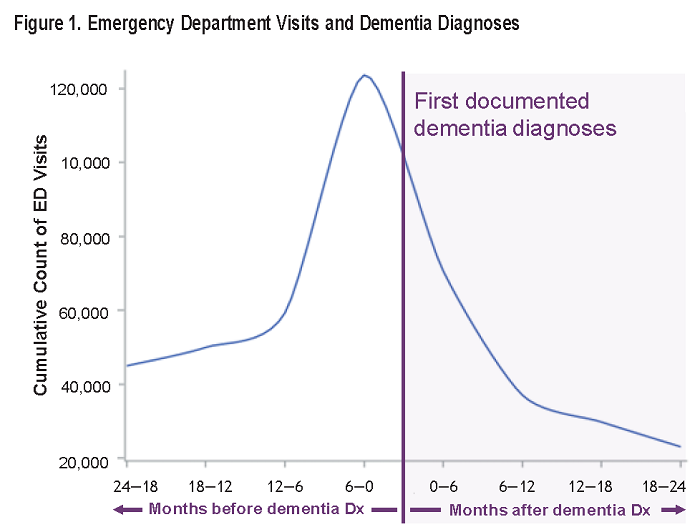
References
|
|