
|
|
Research HighlightThe Changing Landscape of Veteran Emergency Care: Implications for Policy and PracticeKey Points
VA stands at a critical juncture, facing budgetary constraints amidst escalating costs and shifting care paradigms. The dramatic increase in Veterans utilizing community care poses a threat to the integrity of VA’s direct care system, potentially resulting in clinic closures, service reductions, or hiring slowdowns if not addressed. VA spending on community care surged from $7.9 billion in 2014 to $18.5 billion in 2021, now constituting a third of the medical care budget. This increase raises valid concerns about the program’s long-term sustainability. Notably, emergency care represents the largest portion of this expenditure, encompassing over one third of the total community care budget. Challenges and Considerations in Emergency Care. Accessing emergency care within the VA system presents challenges for many Veterans, especially those in rural or underserved areas, due to the limited geographic coverage of VA emergency care facilities. Consequently, Veterans often turn to community emergency departments (EDs). Implementation of the MISSION Act and concomitant changes in emergency care payment authorities, notification processes, and reimbursement rates have also simplified the process of approving and paying for community emergency care. In turn, VA has witnessed an unprecedented surge in demand for community-based emergency care, which has emerged as the primary contributor to VA community care spending, with community ED visit expenditures rising by 46 percent since 2020. Insights from a Recent Study. In our retrospective analysis spanning from 2016 to 2022, we found the annual number of community ED visits increased 154 percent, from 465,253 in 2016 to 1,180,106 in 2022, while the number of unique users of community emergency care increased by 134 percent, despite a relatively stable Veteran population.1 The proportion of all ED visits that occurred in the community versus VA progressively increased from 18 percent to 37 percent during this time. Total community care ED payments, adjusted to 2021 dollars, rose from $1.18 billion in 2016 to $6.15 billion in 2022. These costs, driven primarily by rising admission rates, underscore the evolving landscape of emergency care utilization among Veterans. Notably, conditions such as septicemia, heart failure, acute myocardial infarction, stroke, and COVID-19 were among the top reasons for community emergency visits resulting in admission, while conditions with the highest charges were hip fractures, conduction disorders, and septicemia. The observed surge in community care ED visit costs may be partially attributed to demographic shifts, particularly the increasing proportion of elderly Veterans, who may present a higher burden of illness. One explanation for the surge in costs related to community emergency care could be attributed to a phenomenon known as payer-shifting, a concept supported by prior research.2 MISSION Act-related changes in payment and notifications, particularly reimbursing most community ED claims at 100 percent of Medicare rates, may have inadvertently created incentives leading to a transition in the primary payer for emergency care. This shift, from Medicare or other private payers to VA, has critical implications and raises the question of whether payer-shifting is primarily associated with patient choices or clinician practices, an issue warranting further research. Nevertheless, the rise in community emergency care use is significant given prior research indicating that Veterans have historically been hesitant to embrace community-based emergency care.3 The juxtaposition of these findings underscores the need for further investigation into the factors influencing Veterans’ healthcare- seeking behaviors, as it is conceivable that as Veterans feel more comfortable seeking care in the community, community care ED utilization may continue to rise. Variations in Care Settings and Patient Needs. Our analysis unveiled noteworthy variations in the types of conditions treated in community versus VA EDs. Veterans appeared to utilize community EDs for more acute reasons, with conditions such as cardiac arrest, stroke, and sepsis featuring prominently. In contrast, over 80 percent of low back pain, other musculoskeletal pain, and upper respiratory illnesses are treated in VA EDs. Proximity to community ED facilities may influence the choice of care settings, particularly for emergencies requiring timely interventions. Regional and Facility-Level Dynamics. On average, VA facilities purchased 22 percent of ED visits from the community, which increased from 14 percent in 2016 to 32 percent by 2022. Facility-level analyses found associations between facility characteristics and the proportion of emergency care purchased in the community. Lower complexity and higher volume facilities were more likely to purchase emergency care from community providers, underscoring regional differences in care delivery. Potential Solutions. As VA policy makers grapple with the explosion in emergency care use and costs, they are considering strategies like repatriation, which involves transferring Veterans from community settings to VA facilities after initial stabilization and treatment. This approach carries several potential advantages, such as mitigating care fragmentation and theoretically decreasing costs by capitalizing on VA’s comprehensive medical records, and reducing redundant or unnecessary testing. However, these benefits come with inherent risks, including treatment delays, the possibility of incurring additional expenses related to the cost of transport, and other required resources such as staffing. Additionally, the reimbursement model employed by VA to compensate for community admissions may present challenges in realizing cost savings when repatriating patients from community hospitals back to VA facilities after payment has already been rendered. Also, VA facilities vary significantly in their capacity to accept and treat patients from the community (e.g., bed availability, specialist availability). Finally, the repatriation process itself introduces risks such as infection, airway complications, and cardiac arrest. We recommend that future research examine the cost-benefit analysis of repatriation strategies for Veterans admitted to community hospitals. Our findings underscore a pivotal transformation in the acute care landscape for Veterans, with a pronounced shift toward community-based emergency care, especially following the MISSION Act’s implementation in 2019. While this shift likely signifies an enhancement in access to care, it is essential to recognize its potential unintended repercussions. Notably, increased reliance on community emergency care can lead to concerns regarding healthcare outcomes and care coordination, potentially resulting in fragmented patient experiences across care settings. While VA remains the primary source of emergency care for Veterans, it now operates as both a care source and purchaser, necessitating a thorough evaluation of this transformative shift. Future work should focus on assessing the impact of this shift, particularly on the quality of healthcare services delivered in community settings, including patient satisfaction, and health outcomes. 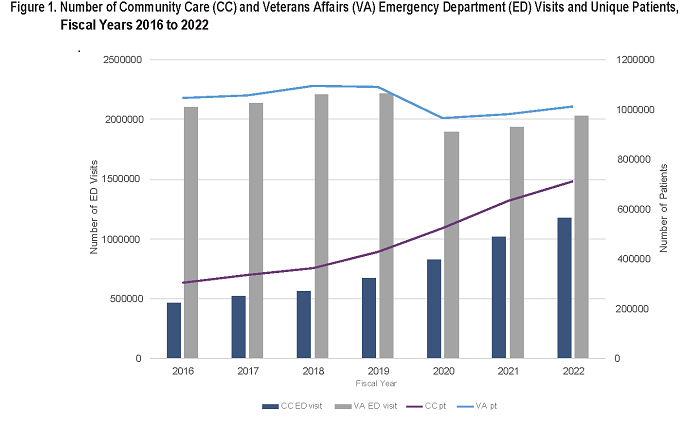
References
|
|