
|
|
CommentaryVA Emergency Medicine: Using Evidence to Inform Policy and Improve Access to Effective Emergency and Urgent Care for VeteransVA Emergency Departments (EDs) and Urgent Care centers (UCs) are responsible for over 2.3 million Veteran clinical encounters annually. As venues for immediate, on-demand access to care for Veterans, VA EDs and UCs stand ready to provide emergent and urgent care during all hours of operation. This includes maintaining a posture of continuous readiness to successfully manage a wide variety of medical, surgical, and behavioral health emergencies. While the above can be said of most emergency and urgent care sites in the United States, VA EDs and UCs are particularly adept at meeting the unique healthcare needs of the Veteran population. For example, we recognize that Veterans tend to be older and have a higher burden of mental health diagnoses than the average U.S. population. Furthermore, many of our Veterans reside in geographically remote areas with limited VA and community healthcare access. It is imperative that we develop a deeper understanding of the ways in which the acute care needs of Veterans differ from the general population, including evaluating strategies, practices, and policies that promote improved healthcare outcomes for Veterans. Indeed, work in this space has already informed us that Veterans transported by ambulance to VA EDs have a significantly lower risk of mortality than Veterans transported to a non-VA ED.1 This finding, in combination with other work demonstrating relatively favorable patient outcomes with VA-based care helps motivate a core strategy to enhance access to high- quality, integrated, and reliable emergency and urgent care for Veterans. As illustrated by the infographic below, the National Emergency Medicine Office (NEMO), which has clinical oversight responsibility for VA EDs, UCs, Emergency Ambulance Services (EAS), and Tele-Emergency Care, views each of the clinical programs under its purview as playing a critical role in enhancing access to immediate medical care for Veterans. While increasing timely access to care is a necessary first step towards promoting positive healthcare outcomes among Veterans suffering from acute illness and injury, further inquiry and investigation is needed to answer critical questions that will drive future policy and strategic investment decisions. To this end, we briefly review some of the key issues within each of the core programmatic areas of VA Emergency Medicine. VA Emergency Departments and Urgent Care CentersVA boasts 110 Emergency Departments across the enterprise, each delivering state of the art emergency care to Veterans 24 hours a day, 7 days a week, 365 days a year. These clinical units are designed to provide care for any complaint, to anyone, at any time. That said, our ability to rapidly evaluate patients is often beleaguered by capacity constraints in which stabilized Veterans awaiting an available inpatient care bed languish in the ED, sometimes for hours or days on end. The practice of holding admitted patients in the ED – often in hallways – while those patients await an available inpatient bed, also known as “inpatient boarding,” has been shown to result in adverse patient outcomes, to increase the risk that patients will leave prior to receiving emergency medical attention, and to contribute to staff burnout.2 Exploring the impact of inpatient boarding on the Veteran population and investigating effective strategies to decrease or mitigate inpatient boarding in the ED is critical. The exceptional care provided through VA EDs would not be possible without the professionalism and dedication of thousands of committed clinical staff members. Unfortunately, there has been a rise of interpersonal violence within U.S. EDs, with 70 percent of emergency nurses, and nearly 50 percent of emergency providers and physicians reporting at least one episode of workplace assault.3,4 It remains unclear to what extent this phenomenon is impacting the VA emergency care workforce, but a better understanding of its prevalence as well as knowledge of effective strategies to mitigate the risk of violence against clinical staff devoted to the care of Veterans is sorely needed. Tele Emergency CareTele Emergency Care is a novel method of allowing Veterans access to a virtual evaluation by an emergency medical provider from the convenience of the Veteran’s home. This service allows Veterans to be directed to receive the right care at the right time and right place. In many instances, Veterans can have their acute care issues addressed and successfully resolved through a virtual evaluation alone. As an emerging modality for immediate care delivery, much information is needed to help inform clinical and policy decisions related to Tele Emergency Care. This includes knowledge about the types of clinical presentations most amenable to successful resolution through a virtual encounter, the ideal professional skillset necessary for effective virtual emergency care, and potential gaps in Veterans’ ability to access virtual emergency and urgent care resources. Indeed, there are many critical operational and clinical questions that need urgent investigation to support safe and effective practice in this novel space. Emergency Ambulance Services (EAS)The ability to transport acutely ill Veterans to and from VA and community sites of care isa critical element of the continuum of care. Unfortunately, VA and community facilities are faced with increasing delays in being able to access ambulance services.5 More information is needed about the clinical impact of such delays along with their root causes. In many instances, VA ambulance services can provide this resource in a much more accessible manner. However, data are still needed to help guide effective EAS policy development, equipment and staffing recommendations, and appropriate clinical protocols to best serve Veterans. Geriatric Emergency CareVA EDs serve predominantly older populations with Veterans aged 65 and older accounting for 54 percent of all ED visits. In recognition of this, VA Emergency Medicine has partnered with the Office of Geriatrics and Extended Care, the American College of Emergency Physicians (ACEP), West Health Institute, and the John A. Hartford Foundation to promote geriatric emergency medicine programming and accreditation. As a healthcare system, VA has the largest number of geriatric-accredited EDs in the nation. Yet we need further dataon Veteran clinical outcomes associated with receiving care in a geriatric-accredited ED, including elucidating programs or initiatives that are particularly impactful in preventing harm or yielding positive health outcomes. While VA Emergency Medicine has advanced significantly since its initial recognition as a specialty program in 2011, we depend on our research partners to evaluate our current policies and programs and to identify exceptional practices that will help inform future strategic decisions. It is only through such a partnership that we can accelerate VA Emergency Medicine’s journey to be the immediate care provider of choice for America’s Veterans. 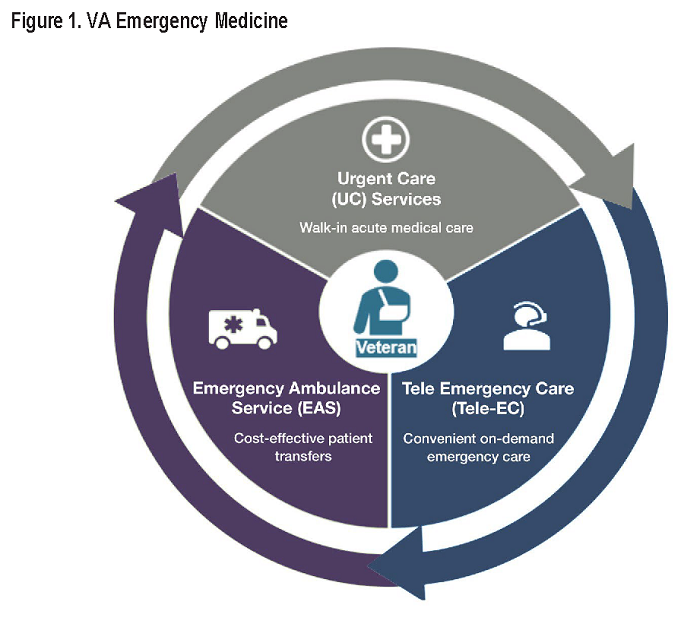
References
|
|
Next ❯