
|
|
Innovation UpdateOptimizing Virtual Modalities in VA to Enhance Healthcare for Women VeteransCare for women Veterans is at a pivotal juncture. In 2020, Congress passed the Deborah Sampson Act, which requires the Veterans Health Administration (VA) to expand support and access to high-quality care for women Veterans.1 A fast growing subpopulation, women Veterans are more diverse and more likely to be single heads of households than their male counterparts. These characteristics have implications for women Veterans’ engagement in their own healthcare.2 Since the 1990s, VA has adapted care to address sex- and gender-based differences in health needs, preferences, and utilization patterns, resulting in increased satisfaction for women and decreased gender-based health disparities. Such adaptations include the establishment of women’s health comprehensive care clinics, identifying designated women’s health providers, and employing women Veteran project managers at every VA Medical Center.3 Yet, women Veterans continue to face unique logistical, cultural, and geographic challenges to receiving necessary healthcare.4 To overcome these barriers, VA needs to explore innovative means of providing care to women Veterans. Virtual care offers one such potential approach for women Veterans, who have already demonstrated eager uptake of virtual modalities, both before and during the COVID-19 pandemic.5 Our project, CompreHEnsive ViRtual Care for WOmen VEteranS (HEROES), seeks to identify barriers and facilitators to virtual, patient-centered VA healthcare for women Veterans and to implement strategies for optimizing its delivery. Our goal for HEROES is to generate an equity-focused guide that VA can integrate into existing and evolving telehealth infrastructures. To ensure sustainable solutions, we are working with a diverse team of health researchers, clinicians, and women Veteran patients. This four-year study is guided by Public Health Critical Race Praxis. We will employ participatory methods (e.g., Delphi method, human-centered design) to create a novel Implementation Blueprint. This blueprint maps evidence-based actionable steps that women’s health programs can use to guide how and when to deliver virtual care that promotes engagement and quality. We will then evaluate the blueprint and identify areas for further adaptation through a multiple methods evaluation. 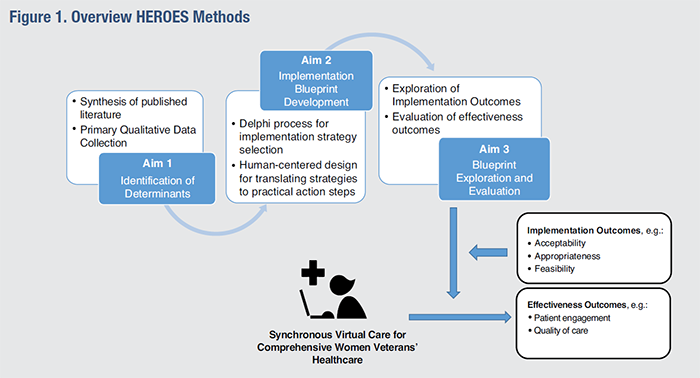
|
|