
|
|
CommentaryImproving Access to High-Quality VA Care: MISSION Act ReadyThe Office of Veterans Access to Care (OVAC) is committed to the oversight and support of access in VA. A range of factors affects access to care in VA, from MISSION Act eligibility for community care to meeting the urgent needs of Veterans to the implementation of a more comprehensive electronic health record (EHR). Future opportunities for research are needed to understand how best to improve upon access efforts over the coming years. MISSION ActVA has been buying and providing community care for Veterans since 1945. The passage of the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act in June 2018 consolidates community care into one permanent program. VA is not privatizing but continuing to put Veterans at the center of their healthcare by giving them a choice. The MISSION Act’s access standards for eligibility that went into place in June 2019 offer Veterans a choice for community care if wait times for an appointment in VA primary care and mental health are greater than 20 days and greater than 28 days for specialty care. In addition, the standards include eligibility if a Veteran drives more than 30 minutes for a primary care or mental health appointment—or 60 minutes for a specialty care appointment. Moreover, if a provider and Veteran agree that it is in the best interest of the Veteran to receive community care even if the VA facility is meeting all standards, the Veteran is eligible to do so. The MISSION Act also calls for development of a program in facilities with medically underserved populations. Thus far, we have worked in primary care and mental health to identify underserved sites using a robust module. ICEPThe OVAC is collaborating with the Office of Clinical Operations, Community Care, and others to lead improvement efforts in access with the Increasing Capacity, Efficiency, and Productivity (ICEP) initiative. This initiative is aimed at improving access in primary care, mental health, and specialty care to get facilities “MISSION Act Ready” for access standards implementation in June 2019 and continuing to improve over time. Because evidence supports VA as the best choice for Veteran healthcare, this initiative enables increased care in VA. When considering wait times and quality measures, VA compares favorably to the community. Wait times over the past few years in the community have shown little improvement. In fact, a recent JAMA Network Open study found that the mean overall wait time in VA was 12 days shorter compared to wait times in the community in 2017.1 Average wait times in VA have improved by 4.92 days from 2014 to 2017, while the private sector showed no improvement. The JAMA study points to VA’s efforts to improve access through reducing wait times in recent years. A recent RAND study found that VA demonstrated a higher quality of care compared to the private sector.2 Also, mental healthcare in VA proves to be better for Veterans’ needs than the private sector.3 Overall, VA healthcare exceeds private-sector care in quality and timeliness and is the best choice for Veterans in many circumstances. The ICEP initiative is building on the momentum of these achievements, preparing facilities to become MISSION Ready. The first phase of the initiative began in January 2019 with a focus on ensuring accurate expected time in clinical activities to actual time in clinical activities for providers. With support from other VA program offices, OVAC has provided training to all VA medical centers that includes strategies proven to improve capacity, efficiency, and productivity, and to increase the time VA providers are conducting direct patient care. We continue to identify sites that do not meet the access wait times standards and support review of core processes, whether it be additional staff, space, or a way to align clinic grids. As of March 2019, 68.5 percent of primary care sites have average wait times for new patients of less than or equal to 20 days, with 98.6 percent in mental health. It is expected that the number of sites meeting the standards will continue to rise. Specialty care also is trending toward improvements in waiting times for new patients of less than 28 days. For example, 86 percent of sites are meeting MISSION standards for average new patient wait times of less than 28 days in cardiology as of March 2019. Many sites have received virtual one-on-one site visits to review capacity data, offer suggestions, and develop strategies for improvement, with action plans to increase the number of appointments for Veterans to be seen. Phase 2 of ICEP will focus on strategies to improve access including, but not limited to, increasing the use of non-traditional care (i.e., electronic consults from primary care to specialty care, VA Video Connect-virtual appointments on a phone or tablet), utilizing nursing staff effectively, and discharging patients from specialty care back to primary care. The ICEP initiative will provide networks and medical centers with a menu of strategies to support improvement. The third phase of ICEP will focus on recapturing appointments being sent to the community by implementing longer-term national and regional strategies. In partnership with the Office of Community Care, OVAC will identify medical centers with the highest volume of community care to prioritize resources. Additional strategies to increase access are currently under review. Leading healthcare systems provide clinical contact centers that offer urgent healthcare needs via video and telephone calls. In addition, all 18 VA networks have Clinical Resource Hubs that provide primary care and/or mental healthcare via virtual appointments. The addition of specialty care and clinical pharmacy specialists is planned. MISSION will put decision-making about where to receive care squarely in the providers’ hands. Providers will use a new application called the Decision Support Tool (DST), developed by the Office of Community Care, to inform providers and patients about eligibility for Community Care at the time they are discussing care plans with patients. The DST will guide informed decisions about the use of VA and/or Community Care resources. Same Day ServicesVA has taken many steps to modernize our approach to scheduling appointments and consults that have resulted in shorter wait times and improved access to high-quality care. As of December 2017, OVAC achieved same-day services in primary care and mental health at all VA medical centers and community-based outpatient clinics nationwide, enhancing access for all Veterans by providing them with timely care. Same-day service means VA will respond to Veterans’ requests right away. This includes things like authorizing a medication refill, answering a health-related question via phone or email, providing a nurse visit, administering walk-in vaccinations, or resolving issues with a medical device/equipment. Ongoing trainings and further education are under development to support frontline teams in providing same day services. Electronic Health Record ModernizationThe Electronic Health Record Modernization (EHRM) project entails implementation of Cerner commercial off-the-shelf solutions, which will provide an accurate and comprehensive health record at the point of care, resulting in improved patient care and safety. The integrated scheduling solutions will allow VA to better manage supply and demand, thus improving access for Veterans. To date, the EHRM Councils and Workgroups, consisting of field experts within VA who can act as Solution Subject Matter Experts, have completed five of eight workshops. The plan is to go-live at the Initial Operating Capability (IOC) sites, Puget Sound, American Lake, and Spokane, in March 2020. 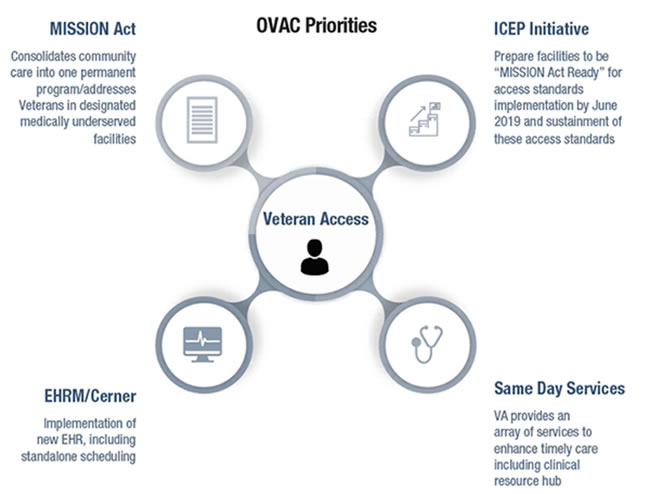
Future Research OpportunitiesA multitude of new VA access initiatives, including the MISSION Act, create the perfect environment for rich partnerships between operations and research. Robust statistical analysis guided the identification of underserved facilities and the development of the new access standards, strengthening OVAC’s relationship to researchers in the process. Moreover, researchers are already developing protocols to evaluate upcoming MISSION Act interventions, such as a medical scribes pilot program to improve productivity, and the deployment of mobile clinics to improve access to care in underserved areas. The role of VA research will only grow in the future, expanding beyond the MISSION Act and into other OVAC-led initiatives to improve access to care and productivity. VA remains committed to ensuring that Veterans receive the highest quality care. VA’s long history of working with patients has set it apart from the private sector with its ability to address the specialized needs of Veterans. The MISSION Act will build on the foundation VA has set for utilizing community care when needed—and is not an effort to privatize. The goal is to keep Veterans within VA and only send them to the community when access standards cannot be met. Through numerous ongoing initiatives at VA, specifically OVAC, we are continuing to improve access at VA and become MISSION Ready. Reference
|
|
Next ❯