November 22, 2023

In any healthcare organization, nurses span the entire care continuum and are involved in virtually every aspect of patient care. Given that VA is the largest employer of nurses nationally and has highly valuable data on nurses, VA is in the unique position to set the standard for nursing care. To fully ensure that those standards are well-informed, establishing a current nursing research agenda is vital.
In November 2023, VA Health Services Research and Development Service, with VA’s Office of Nursing Services, brought together clinical stakeholders and researchers to review the State of the Art in Nursing Research (SOTA). Taking part in SOTA were representatives from research both within and outside of VA, VA program offices, and clinical leaders from throughout the country.
Goals of the SOTA included:
Results from this intensive, two-day conference will include:
For More Information
To learn more about the Nursing Research Agenda SOTA, or about nursing research in VA, please contact Amelia Schlak (Amelia.Schlak@va.gov) or Sheila Sullivan (sheila.sullivan2@va.gov).

Nursing SOTA participants
October 19, 2023
By Hayden Bosworth, PhD

Hayden Bosworth, PhD
I think it’s important for any investigator to understand how research and mentoring should inform each other, and I hope this note offers a valuable discussion of that relationship. Many chronic conditions that Veterans experience have common threads including causes, treatments, and outcomes. Focusing on those commonalities allows VA researchers and clinicians of many specialties to address these issues in tandem. While our research needs to answer feasible, operational, specific questions, mentoring allows for a broader, more encompassing perspective, with the overall goal of improving Veteran health outcomes.
Answers to questions including: how do we reduce clinical inertia and use extended members of the healthcare team to improve cardiometabolic outcomes (IIR 08-297); how can telehealth use improve access to care for those with cardiovascular disease (IIR 04-426): how do we address care coordination among Veterans with comorbid HIV and hypertension (IIR 19-418); and how do we reduce cardiovascular inequities among rural African American and women Veterans ultimately lead to direct impact on Veterans’ care. These questions are an outgrowth of mentoring clinicians with diverse backgrounds including endocrinology, nephrology, aging, cardiology, internal/family medicine, and nursing.
Working with, and mentoring, diverse clinicians has helped me to better understand the factors that contribute to the many conditions Veterans experience. Mentoring also helps us understand the multifactorial challenges and concerns that contribute to Veterans’ health. For example, Veterans may have difficulty following treatments (e.g., medication adherence, exercise, weight management). Providers should consider how care coordination and clinical therapeutics can impact Veterans. It’s also important to reflect on how barriers within the healthcare system, such as access to care, can impact the provision of high-quality care. We also need to consider how policy may influence where and how Veterans obtain care. Lastly, in addition to a multifactorial perspective, we must take into account unmet social needs, such as material circumstances (e.g., access to healthy food); behavioral factors (e.g., diet, exercise, smoking); and psychosocial factors (e.g., stressors, social isolation).
I have found that mentoring diverse clinicians of different backgrounds and training allows for a more inclusive gathering of knowledge and expertise. Hence, providing multiple pathways ensures improved Veteran healthcare outcomes.
It is my philosophy that mentoring the next generation of clinical researchers is essential if we want to ensure our Veterans receive the quality of care they deserve. Mentorship pulls the next generation into this process of considering multifactorial needs and common underlying causes in a collaborative process. Mentorship also allows us to model this collaborative approach to research and care delivery for our Veterans.
In summary, the role of mentorship in clinical research is critical for several reasons – mentorship provides a platform to transfer knowledge, experience, and skills. Serving as a mentor can lead to great professional satisfaction while simultaneously helping mentees navigate their careers, solve research problems, and achieve their goals. Mentees bring fresh perspectives and innovative approaches to research. Mentorship also provides an avenue to promote diversity and inclusion by supporting and guiding individuals from diverse backgrounds. The impact of our guidance and mentorship can extend far beyond our own career, hopefully shaping the research landscape for years to come through the achievements of our mentees. It is my firm belief that supporting our mentees to conduct high-quality research ultimately contributes to better healthcare practices and advancements in science.
September 15, 2023
By Charlesnika T. Evans, PhD, MPH

Charlesnika T. Evans, PhD, MPH
Growing up in Chicago, most of my family members and peers didn’t express interest in topics like archaeology or astronomy. I tended to be the only one in my core group of friends reading dystopian science fiction and fantasy. As a microbiology undergraduate major at the University of Illinois, Champaign-Urbana, I was often exploring unique paths, where I loved taking Religion 101: The Bible as Literature and spending a semester working in Dr. Kakoma’s Microbiology lab in the College of Veterinary Medicine.
The next stop after undergrad was the MPH program at the University of Illinois, Chicago. I was really interested in infectious disease after completing my MPH in 1999, but the pragmatic need for a job landed me on the path of a project manager position for Dr. Fran Weaver on the VA Spinal Cord Injury Quality Enhancement Research Initiative (SCI QUERI) at the VA HSR&D Center at Hines (now known as CINCCH). This initiative was focused on improving implementation of evidence-based practice and care for Veterans with SCI. This experience expanded my knowledge base of SCI including learning how VA was (and continues to be) the largest provider of care for people with SCI in the United States and that people with SCI experienced many secondary complications because of their injury. This path taken led me to learning that infections were one of the most common comorbid conditions in people with SCI. And in fact, very little research had been conducted on assessing the epidemiology, prevention, and management of healthcare-associated infections (HAIs) and antimicrobial resistance in this patient population. This led me to seek a new journey: a return to school for a PhD in epidemiology. I focused my dissertation on looking at bloodstream infections in Veterans with SCI and the impact of inadequate or inappropriate antibiotic prescribing on outcomes. This led me to further work during a funded postdoctoral fellowship through the Paralyzed Veterans of America where I studied SCI provider knowledge, attitudes, and behaviors on antibiotics and antibiotic resistance. This path of working on SCI QUERI, unexpectedly, led me to doing the work I really wanted to do, which was conducting impactful studies on infections in Veterans with SCI.
The next step should have been an HSR&D Career Development Award (CDA), but I was unsuccessful at receiving funding for a CDA. Even though I had a supportive mentor, this traditional path of a CDA to an independent scientist was a blocked road. However, another way to a new road opened to support VA’s mission to improve the diagnosis and management of Veterans injured with mild traumatic brain injury (TBI) during Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OF). As a doctoral level trained epidemiologist, I was able to collaborate with other researchers and serve as a methodologist on several projects on TBI including a VA Service Directed Research (SDR) focused on evaluating VA’s TBI screening program led by Dr. Bridget Smith. I was also able to leverage that failed CDA idea, focus it on Veterans with SCI, and ultimately get an IIR funded on the treatment and management of Clostridioides difficile infection.
These alternative paths have given me the opportunity to work with operational partners such as the VA Spinal Cord Injuries and Disorders National Program Office and the VA Multidrug Resistant Organism (MDRO) Program Office as well as outstanding health services researchers such as Dr. Katie Suda and Dr. Robin Jump. These paths have led me to currently co-leading the VA Combatting Antimicrobial Resistance through Rapid Implementation of Available Guidelines and Evidence (CARRIAGE II) QUERI Program with Drs. Mike Rubin, Makoto Jones, and Eli Perencevich, which is focused on implementing strategies to improve use of antibiotics and prevent healthcare-associated infections.
We can’t all follow a traditional path and that’s ok. Sometimes the road less traveled can still get you there.
August 25, 2023
By Courtney Van Houtven, PhD, MSc

Courtney Van Houtven, PhD, MSc
Many of us have Veteran connections and caregiving stories in our own families that motivate our research for caregivers in the VA setting. With Veteran family members—and as caregiver to a sister living with intellectual disabilities—I experienced the incredible, yet invisible, backbone of support that family caregivers provide to our healthcare systems and society overall. In the U.S., there are approximately 53 million “informal” (friends or family) caregivers who provide in-home help. Of those, approximately 5.5 million are caregivers for Veterans. As a health economics researcher, I was drawn to questions about caregiving and long-term services and supports: Who are these caregivers? What are the causal effects of caregiving for both caregivers and their Veterans? What supports are needed to improve patient and caregiver outcomes? I joined HSR&D 20 years ago to explore these questions and translate the findings into VA policy and operations.
Through my journey at HSR&D—starting as a Career Development Awardee (CDA), and now, as a Research Career Scientist—I have been able to develop research programs that support the mission of the most comprehensive, publicly-funded caregiver support programs in the country—all of it within VA. I began by surveying family caregivers of Veterans in order to discover what training they felt they needed and weren’t getting, and how that training should best be delivered. Over the years, this led to the development and testing of a caregiver skills training program, which evolved from a single site to national, VA-wide adoption.
In an HSR&D funded randomized controlled trial, our team examined a program of supporting and training family caregivers that showed improvements in caregiver and patient experiences of VA care and reported reduced feelings of isolation. Because this training improved an important metric of care quality (experience with care), and addressed persistent gaps in caregiver group training that existed at the time, the VA Caregiver Support Program endorsed the expansion of this caregiver training intervention to more VA medical centers. That led me to new territory, joining forces with implementation scientists as part of a VA Quality Enhancement Research Initiative, which was established to accelerate research evidence into practice. At eight VA medical centers, our amazing team trained 65 staff members who then delivered the caregiver training to 241 caregivers. Based on ongoing demand for caregiver training and high program satisfaction from caregivers, the VA Caregiver Support Program endorsed this intervention (now called Caregivers FIRST) for widespread adoption. Currently, over 125 VA medical centers are running Caregivers FIRST with approximately 3,600 caregivers trained. Few evidence-based caregiver support interventions have been scaled for widespread dissemination, so I am excited to be part of a program that began its inception at VA and became a pragmatic trial that will lead to the development of resource-efficient approaches to support VA in spreading and sustaining this caregiver training intervention.
Over the years, I have seen the immense value of partnered research in scalability. I’ve learned the value in pitching these pragmatic, emergent programs to decision-makers where filling unmet needs may be the “business case.” When our research questions align with decision-maker needs (e.g., performance metrics), partnered research can make a real difference in creating a more caregiver-friendly health system. This is what motivates me to continue to answer these questions to help improve the lives of Veterans and the people who care for them.
July 14, 2023
Christine W. Hartmann, PhD

Christine W. Hartmann, PhD
As an early career researcher, I knew few people outside the building where I worked. I learned about my field and identified opportunities for interesting research, but I was new to VA and to health services research and lacked a social network to test ideas on. At that time, two statements from my mentor, “You need to meet the VA leadership in DC,” and “Let me introduce you to researchers who have similar interests,” changed the trajectory of my career. My research expanded and accelerated by building relationships with VA Central Office policy makers and fellow researchers and staff interested in nursing home quality of care.
From the beginning of my HSR&D career development award, I flew yearly to DC to meet with leaders in the Office of Geriatrics and Extended Care. I currently meet with these folks mostly via Teams; many of them no longer even work in the DC area. But even now, I use opportunities at conferences to connect in person and find value in face-to-face time. I also built partnerships across the country, most meaningfully with my fifteen-year-long research partner, Lynn Snow, PhD from the Tuscaloosa VA. She and I co-constructed a portfolio of research that advances the mission of the Office of Geriatrics and Extended Care and implements a new model of individualizing nursing home care nationwide.
That story began with an HSR&D pilot grant to explore VA Community Living Center (nursing home) care practices and a subsequent HSR&D Merit award to investigate individualized care in Community Living Centers (CLCs). During that time, in addition to phone calls and emails, Lynn and I made once-a-year trips to DC to update Office leadership on findings and collaborate on next steps. We both will never forget sitting at a conference table at a 2016 meeting when the director of Community Living Centers asked us, “What would it take to roll your study’s program out nationally?” Lynn and I almost fell out of our seats. The following year, the Office expanded our intervention to all 134 Community Living Centers. They created a national center to support this effort, the CLCs’ Ongoing National Center for Enhancing Resources and Training (CONCERT), with a terrific field-based team and Lynn and me as co-directors. The Office funded CONCERT continuously through 2021 with over $7 million. In 2021, VA’s Facility Based Care Modernization Plan moved CONCERT into the Office of Geriatrics and Extended Care. Now, nine amazing full-time Office staff run CONCERT for the nation’s 134 Community Living Centers and 151 State Veterans’ Homes.
This journey may sound straightforward, even relatively easy, in the telling. Yet the principle of intermittent reinforcement—delivery of a reward at irregular intervals, which is the strongest motivator for performance—looms large throughout this ongoing research-into-practice adventure. Some of our grant submissions are not funded. Others are. Previously funded trajectories of research peter out because they have little effect on patient care. Others succeed. Team composition shifts over time. Our operational partners become friends and then retire or otherwise leave their positions. The Office completely reorganizes its organizational structure periodically. Balancing the demands of an operational partnership (rapid, changing timelines) with traditional research (slow, relatively inflexible goals) proves difficult. We have a wonderful community of like-minded colleagues invested in the journey. We also struggle with overwork.
The CONCERT program, too, struggled with numerous hurdles. Some years, we almost lost our funding due to administrative snafus or shifts in Congressional priorities. In 2018, front-page newspaper stories about a “quality crisis” in VA nursing homes necessitated major changes to the program’s direction. And the COVID-19 pandemic hit just after NIH-funded work (designed to move this successful program into community nursing homes) began, meaning we had to completely overhaul our training plans.
The research-to-practice road is bumpy. But, intermittently reinforced, we have enough success to keep going. And the relationships we build along the way—with research team members, consultants, operational partners, and the staff and Veterans working and living in the nursing homes—sustain our resolve and make all the effort worthwhile.
Meeting people, making introductions, building relationships. In the end, that’s what grows and gives meaning to my career.
June 21, 2023
By Mary Jo V. Pugh, PhD, RN

Mary Jo V. Pugh, PhD, RN
When I started working for HSR&D as a data analyst at the Bedford Center of Excellence in 1999, I had no idea what I was getting into. I was a freshly minted PhD in developmental psychology and didn’t even know there was a field called health services research. It turned out that my mentor, Dan Berlowitz, MD, MPH, had a vision for the potential of leveraging my background as an Air Force Nurse and longitudinal methodology to develop and conduct innovative health services research. The opportunities provided in my post-doc and Merit Review Entry Program—an early version of the CDA—made me what I am today. What I have learned over nearly 25 years is that when you get an opportunity—and there will be many—take that opportunity by the horns and run!
As a Veteran with a history of military traumatic brain injury (TBI), and the spouse of a Veteran with Gulf War Illness, I developed a research program focused on long-term outcomes of military exposures including TBI. I support the DoD and VA missions to understand and address the impact of TBI within the Long-term Impact of Military Related TBI Consortium (LIMBIC) as lead of the Data and Biostatistics Core and PI of the Phenotype study. This study is going on its 10th year and includes prospectively collected neuroimaging, biomarker, and clinical data from over 2,600 deployed Veterans, and merged DoD and VA health system data. LIMBIC’s goal is to develop interventions to reduce morbidity and mortality in Service Members and Veterans with TBI. Data from this national consortium has resulted in over 100 peer reviewed papers and is making a significant impact on both science and quality of care for Veterans with TBI. An example is a recent paper from our phenotype study that includes ~2.5 million post-9/11 era Veterans, that found that TBI is a risk factor for cardiovascular disease, which is the top cause of death globally and which can be addressed by primary prevention. Another paper focused on mortality associated with TBI was covered in a 3-part series on TBI and suicide in military Veterans by military reporters who received the Gerald R. Ford Presidential Foundation's Honorable Mention for Distinguished Reporting on National Defense.
A more recent opportunity that I am extremely enthusiastic about is evaluation science. My team was given an opportunity to conduct an evaluation to address a VA requirement from the 2021 National Defense Authorization Act. We were able to provide important information on differences in labor force participation and employment for post-9/11 women Veterans and characteristics that were associated with more positive (and negative) outcomes using diverse data. During this process I developed relationships that will last a lifetime and new collaborations that made me think about the world differently. It also stimulated my passion for evaluation because we can make meaningful impact on how care is provided faster than with traditional research models. Since that time my team submitted a successful application for an Evidence Based Policy Center (Strategic Policy Evidence-Based Evaluation Center [SALIENT]). We work collaboratively within our team and with other centers to use data for good. That is all I wanted to do when I joined VA, and I have been fortunate to have the opportunity to do just that!
May 17, 2023
By Stefanie Gidmark, MPH, QUERI Program Specialist

Stefanie Gidmark, MPH, QUERI Program Specialist
As I get close to my 6-month anniversary with HSR&D/QUERI serving as QUERI Program Specialist, I am so thankful to be back with VHA, specifically as a part of the HSR&D community. I started my career with VHA, spending over 8 years as a research project manager based out of the Providence VAMC. I worked on several HSR&D research projects across the years, as well as being an early member of the operationally funded Geriatrics and Extended Care Data & Analysis Center. Leaving in 2019 was a difficult decision, but between the difficulties of remote work within VHA at that time, and the opportunity to challenge and grow my professional skillset while contributing to my local community drew me to other opportunities.
After leaving VHA, I worked at a local (Central Illinois) non-profit healthcare system with a focus on provision of community mental health services. I spent several years in a split position as a Manger of Grants and Program Director for an Emergency Department-based Substance Use Intervention program. Between these roles, I was responsible for securing federal, state, and non-profit programmatic grant funding, leading implementation efforts of evidence-based practices, and ensuring state and regulatory award compliance. It was a rewarding experience which gave me a deep appreciation for the complexities and struggles of implementing new processes in health care settings and developing mechanisms to improve processes across the full grant lifecycle. Despite the many great attributes of that work, I continued to miss VHA, specifically the HSR&D community. I am incredibly thankful for VHA’s adoption of remote work policies that allowed me to come back despite my physical location in rural Illinois.
Serving as QUERI Program Specialist allows me to draw on the knowledge and skills I learned working in the field with VHA, and in community healthcare settings to help improve the quality of care for Veterans. I am very fortunate to get to engage with investigators and program teams to support their important work. I am excited to continue to learn how to best support our Centers and improve our internal processes to better meet the dynamic needs of the field.
April 12, 2023
By Cathie Plouzek, PhD, Scientific Program Manager
As part of the ORD reorganization, the Pain/Opioid Actively Managed Portfolio (POp AMP) has been established as a shared cross-service portfolio. The focus of the POp AMP will be to review preclinical, translational, clinical, and health services/implementation research applications where pain and opioid use, and the consequences of opioid use, are the primary outcome(s) of the study. The POp AMP will release two merit Request For Applications (RFAs) in mid-April that will be posted on the RFA page of the ORD intranet site at https://vaww.research.va.gov/funding/rfa.cfm (If you have VA network access, copy and paste the URL into your browser.).
A Pre-application is required for both RFAs and must be submitted through eRA. The due date for the Pre-application for the Summer RR&D and HSR&D review round is May 1. Applications follow the general service timelines (Spring/Fall for BLR&D and CSR&D, and Summer/Winter for HSR&D and RR&D oriented applications); however, they may not have the exact deadlines as the other Parent RFAs in all services. Please check the due dates in the POp AMP RFAs.
Register for the Cyberseminar on Tuesday April 18, at 2-3 pm ET to hear more about these new RFAs.
March 14, 2023

Christopher Bever, MD, MBA
Deputy CRADO for Investigators, Scientific Review, and Management
By Christopher Bever, MD, MBA, Deputy CRADO for Investigators, Scientific Review, and Management
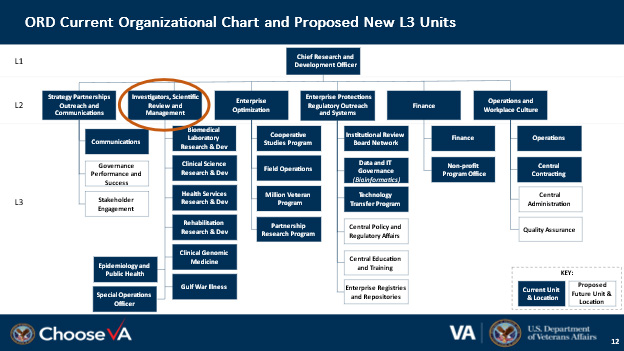
The Enterprise Transformation Initiative: VA, led by the Office of Enterprise Integration, has embarked on a transformation to support better integration across the organization to provide better services to Veterans. Following this lead, the Office of Research and Development (ORD) is undergoing a transformation to better integrate research across the organization. As part of this process, the ORD Services (Rehabilitation R&D, Health Services R&D, Clinical Science R&D, and Biomedical Laboratory R&D) are being combined into a new organization: Investigators, Scientific Review and Management (see below).
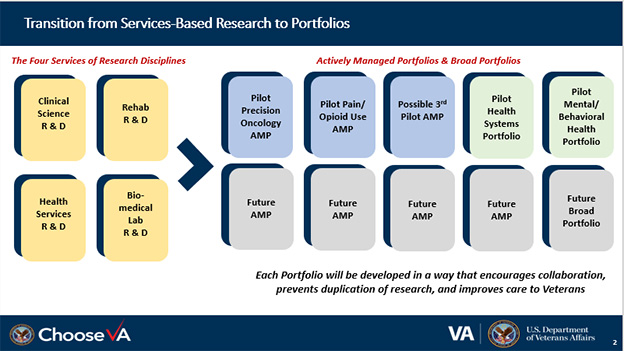
Organizing VA research funding around the needs of Veterans: An important part of the enterprise transformation will be to shift funding from portfolios related to research disciplines and methods to portfolios of Veteran need, such as Precision Oncology, Pain and Opioid Use Disorders, Health Services and Behavioral and Mental Health, Traumatic Brain Injury, Suicide Prevention, Gulf War Illness, and Military-related Exposures. Importantly, this will enhance integration of research across disciplines, support collaboration with our VA clinical program office partners and other important stakeholders, facilitate the translation of VA research to clinical care and show Congress and other important stakeholders how the research appropriation is being used to address the health needs of Veterans. While the final design of the new portfolio organization has not been determined, it is likely to be a combination of focused portfolios [also referred to as actively managed portfolios (AMPs) (i.e., suicide prevention)] and broad portfolios (i.e., behavioral and mental health).
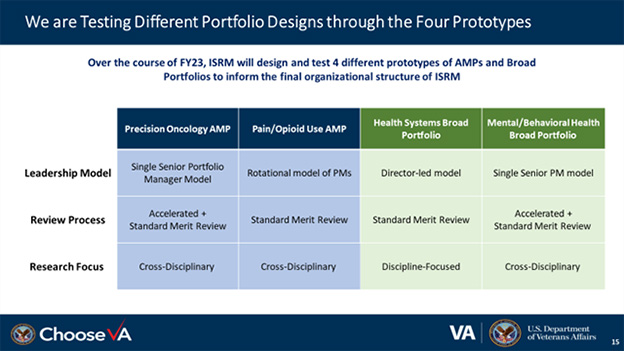
A year of designing and testing: The transition to portfolios of Veteran need poses a number of challenges which require a period of iterative designing and testing. How to best organize the managed portfolios must be determined and we are currently in the process of pilot testing several different AMPs (see the figure below). We are testing out an AMP led by a senior portfolio manager and an AMP led by a team of portfolio managers. We are also testing out a new accelerated review process as part of one of the AMPs. We will be doing tabletop modeling in the next few months to determine how to structure the funding decision process in the managed portfolio process and what changes will be needed in the VA financial systems to support this new organizational structure.
How can you help? The health services research community, both in the field and in the Office of Research and Development, has played a key role in the design process by coming forward with helpful suggestions and directly supporting the development and testing process. I look forward to your continued active engagement in this process and welcome your ideas and suggestions on how we do the best job possible with the reorganization and in the process support the growth of the health services research program (including the QUERI program).
February 16, 2023
By Amelia Schlak, PhD, RN, AAAS Science and Technology Policy Fellow

Amelia Schlak, PhD, RN, AAAS Science and Technology Policy Fellow
It was great to meet so many HSR&D and QUERI colleagues at the annual meeting after connecting with several of you over the past seven months. For those I have not had the chance to meet, I am working in HSR&D as a AAAS Science & Technology Policy Fellow on research portfolios focused on nursing, Long COVID, and burnout. As a nurse and health services researcher, I am excited to grow and sponsor research in emerging priority areas.
One such area is nursing. Nurses span the entire care continuum and are involved in virtually every aspect of patient care. VA is also the largest employer of nurses nationally and has unique data on nurses which has largely been untapped so far. To address this, I am working across HSR&D, QUERI, and Rehabilitation R&D to develop a nursing research agenda. As a former VA nurse and as a nursing workforce researcher, I am incredibly excited and grateful to be leading this effort along with experts from the field and the Office of Nursing Services.
To develop a nursing research agenda, we are planning a Nursing State-of-the-Art (SOTA) Conference for Fall/Winter 2023. The Nursing SOTA will bring together VA investigators, external experts, and other stakeholders to set the nursing research agenda. Our SOTA will inform a future RFA on nursing-related issues. For example, we are considering how future research can improve nursing care at the bedside or in the clinic by considering nurse staffing, education, diversity, retention, and other areas. If we have not gotten the chance to connect and you are interested in the nursing research agenda, please reach out and share more about your research and interest in the nursing research agenda.
Another constantly evolving area is COVID-19, and more particularly, Long COVID. In my role, I’ve been working to manage and grow the Long COVID research portfolio and am excited to share that HSR&D is launching the Long COVID Practice-Based Research Network (PBRN). There are currently 23 VA Long COVID clinics (and counting!). The Long COVID PBRN will lead and organize research efforts across these sites, working alongside internal and external VA stakeholders to develop best practices for Long COVID care.
In partnership with another AAAS fellow, Dr. Karen McNamara, I am working to develop burnout and well-being focused research. As much of my own research has focused on nursing burnout and solutions for it, I am excited to help shape the direction of this research in VA. The pandemic has highlighted the untenable circumstances that many individuals face in their workplace. For clinicians, most of these issues were not new, but rather exacerbated by the pandemic. You may have heard of REBOOT, or the VA-wide taskforce working to “Reduce Employee Burnout and Optimize Organizational Thriving” (REBOOT). In alignment with this national effort, HSR&D is working to develop and support research to improve VA workforce outcomes, with particular emphasis on system-wide interventions.
January 17, 2023
By Jessica Cleveland, MSOR, AAAS Science & Technology Policy Fellow
Happy “new calendar year”, everyone. I hope you were able to find time to do what energizes you over these last few weeks, whether that’s being with family, traveling, or just sitting at home enjoying a nice cup of tea or coffee. For those of you I haven’t yet met, I am a AAAS Fellow who joined the HSR&D office in September. Prior to that, I spent the bulk of my career at Dana-Farber Cancer Institute in Boston working in the informatics and analytics space applying systems engineering techniques to the design and implementation of tools for quality improvement and clinical decision support. From building simulation models to redesigning workflows to developing performance measures, my goal has always been to optimize data and technology around clinical practice.
In this fellowship experience I look forward to continuing to be a bridge between research and operations and expanding on my experience from a large academic medical center to better understand VA’s journey in becoming a learning health care system. As part of the ORD realignment (https://vaww.hsrd.research.va.gov/realignment/ - intranet only), I am working on building out the Quality, Safety, and Value (QSV) priority area within the new cross-cutting Health System Portfolio. The new QSV priority area will focus on studies that validate and implement measures of QSV, compare interventions across settings including direct vs community care, as well as studies that aim to understand the organizational context of care and workforce burnout. As part of this effort, I have begun meeting with key offices including the Office of Quality Management, National Center for Patient Safety, and the Office of Analytics and Performance Integration to help identify areas where research could provide the most value in helping them meet their goals or address issues they have identified.

VA Secretary Denis McDonough (left) Jessica Cleveland, MSOR, AAAS Science & Technology Policy Fellow (right)
I am also working to establish pathways for projects within the Office of Health Innovation and Learning (OHIL) to collaborate with researchers when appropriate. For example, there is a growing interest in making Virtual Reality technology part of standard of care. With over 160 VA facilities participating in projects that have numerous clinical use cases and increased Veteran interest (showcased at the recent Veteran eXpeRience event), it is imperative to establish rapid pipelines to study the effectiveness and implementation of these new technologies.
From making awkward small talk with the SecVA as we pose for a holiday picture to flying out to Salt Lake City to meet some of the many distinguished investigators within this system, this fellowship has already been such a rewarding experience. I look forward to partnering with and meeting many more of you in the field as we work together to better understand and deliver the best care to our Nation’s Veterans.